Introduction
Health psychology is an essential subfield within psychology that focuses on understanding how psychological factors influence health and illness. It integrates the fields of psychology and health to promote overall well-being and to understand the psychological mechanisms that underpin health behaviours.
As defined by the American Psychological Association (APA), health psychology examines the interplay of behavioural, cognitive, emotional, social, and biological factors in health and illness (Taylor, 2017).
This comprehensive overview will delve into the definition, aims, and scope of health psychology, providing evidence and citations to support the discussion.
Definition of Health Psychology
Health psychology is the scientific study of how psychological, social, and biological factors affect health and illness. It seeks to understand how people cope with illness and the psychological processes that contribute to health maintenance and disease prevention (Ciccarelli & Meyer, 2006).
5 Important Definitions of Health Psychology
- Ciccarelli & Meyer (2006), health psychology is the scientific study of behaviour and mental processes in relation to health and illness.
- Taylor (2017), health psychology is a branch of psychology that focuses on how biological, social, and psychological factors influence health and illness.
- Matarazzo (1980), health psychology is the aggregate of the specific educational, scientific, and professional contribution of the discipline of psychology to the promotion and maintenance of health, the promotion and treatment of illness, and related dysfunction.
- American Psychological Association (APA), health psychology is a subfield of psychology that focuses on the relationships between behavioural, cognitive, psychophysiological, and social and environmental factors and the establishment, maintenance, and detriment of health.
- Suls & Rothman (2004), health psychology is the study of the interplay between behaviour and health, particularly how psychological factors can influence physical health and the management of illness.
Key Definitions and Concepts
- Behavioural Factors- Health psychology emphasizes the significance of behavioural factors in influencing health outcomes. For instance, behaviours such as diet, physical activity, and adherence to medical recommendations are critical determinants of health (Ogden, 2017).
- Cognitive Factors- Cognitive aspects such as beliefs, attitudes, and perceptions about health play a crucial role in shaping health behaviours. Research indicates that individuals’ beliefs about their susceptibility to illness can significantly influence their health-related actions (Rosenstock, 1974).
- Social Factors- Social influences, including family, peer support, and community resources, impact health behaviours and access to healthcare. For example, social support has been linked to better health outcomes and enhanced coping mechanisms during illness (Cohen & Wills, 1985).
- Biopsychosocial Model- This model posits that health and illness are influenced by an interplay of biological, psychological, and social factors, challenging the traditional biomedical model that focuses solely on biological aspects (Engel, 1977).
- Health Promotion- Health psychology emphasizes the promotion of healthy behaviours and the prevention of illness through education, awareness, and lifestyle modifications. Interventions that promote healthy lifestyle choices can lead to significant health improvements (Sallis et al., 2006).
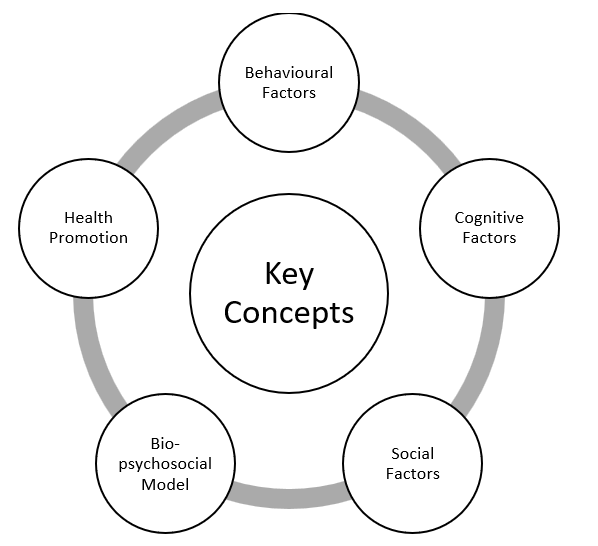
Key Concepts in Health Psychology
Aims of Health Psychology
The aims of health psychology can be categorized into several key areas:
Understanding the Role of Psychological Factors in Health
A primary aim of health psychology is to explore how psychological factors impact health outcomes. This includes-
- Behaviour Change- Health psychologists investigate how thoughts, emotions, and social contexts influence health-related behaviours, such as smoking cessation and dietary choices. For instance, cognitive-behavioural strategies have been effective in promoting behaviour change among individuals with chronic diseases (Kabat-Zinn et al., 1992).
- Coping Mechanisms- Understanding how individuals cope with stress, illness, and medical treatments is vital. Research has shown that effective coping strategies can enhance psychological well-being and improve health outcomes (Folkman & Moskowitz, 2004).
- Mental Health and Physical Health- The interplay between mental health conditions (e.g., anxiety, depression) and physical health is a key focus. Studies have demonstrated that mental health significantly impacts chronic illness management and recovery (Moussavi et al., 2007).
Developing and Evaluating Health Interventions
Health psychology aims to create and assess interventions that promote health and prevent illness. This involves-
- Behavioural Interventions- Designing programs that target specific behaviours can improve health outcomes. For example, interventions aimed at increasing physical activity have shown positive effects on cardiovascular health (Donnelly et al., 2009).
- Psychological Interventions- Implementing psychological strategies, such as mindfulness-based stress reduction, can help individuals manage chronic pain and improve their quality of life (Kabat-Zinn, 1990).
- Health Education- Providing education and resources is essential for empowering individuals to make informed health decisions. Health literacy programs have been effective in enhancing individuals’ understanding of health issues and promoting positive health behaviours (Berkman et al., 2011).
Research and Theory Development
Health psychology contributes to advancing research and theoretical frameworks related to health and behaviour. This includes-
- Conducting Empirical Research- Health psychologists conduct studies to evaluate the effectiveness of interventions and understand health behaviours. For instance, research on the Health Belief Model has provided insights into how beliefs about health risks influence preventive behaviours (Champion & Skinner, 2008).
- Theory Testing and Development- Developing and validating theories that explain psychological influences on health is essential. The Theory of Planned Behaviour, which posits that attitudes, subjective norms, and perceived control influence intentions and behaviours, has been widely applied in health psychology (Ajzen, 1991).
- Identifying Risk and Protective Factors- Understanding the psychological, social, and environmental factors that contribute to health risks or protective behaviours is a critical aim. Research indicates that factors such as self-efficacy and social support can enhance health-promoting behaviours (Bandura, 1997).
Promoting Health Equity
Health psychology addresses health disparities and promotes health equity among different populations. This includes-
- Understanding Social Determinants of Health- Examining how factors like socioeconomic status, race, ethnicity, and access to healthcare influence health outcomes is crucial. The World Health Organization (WHO) emphasizes the importance of addressing social determinants to improve health equity (WHO, 2010).
- Developing Culturally Sensitive Interventions- Creating programs that consider cultural beliefs and practices can enhance their effectiveness. Research shows that culturally tailored interventions are more likely to resonate with diverse populations (Resnicow et al., 2000).
- Advocating for Policy Change- Health psychologists engage in advocacy efforts to promote policies that improve access to healthcare and address social determinants of health. Advocacy for public health initiatives can lead to significant improvements in population health (Satcher, 2006).
Enhancing Patient Care and Healthcare Systems
Health psychology aims to improve patient care and healthcare delivery systems. This involves-
- Patient-centred Care- Promoting approaches that prioritize patients’ psychological needs and preferences is vital. Patient-entered care has been associated with better patient satisfaction and health outcomes (McCormack et al., 2010).
- Interdisciplinary Collaboration- Health psychologists work alongside healthcare professionals to create integrated care models addressing both physical and psychological aspects of health. Collaborative approaches can enhance the effectiveness of treatment (Wagner et al., 2001).
- Improving Healthcare Communication- Developing effective communication strategies between patients and healthcare providers is essential for enhancing understanding and adherence to treatment plans. Research has shown that effective communication improves health outcomes and patient satisfaction (Stewart et al., 2000).
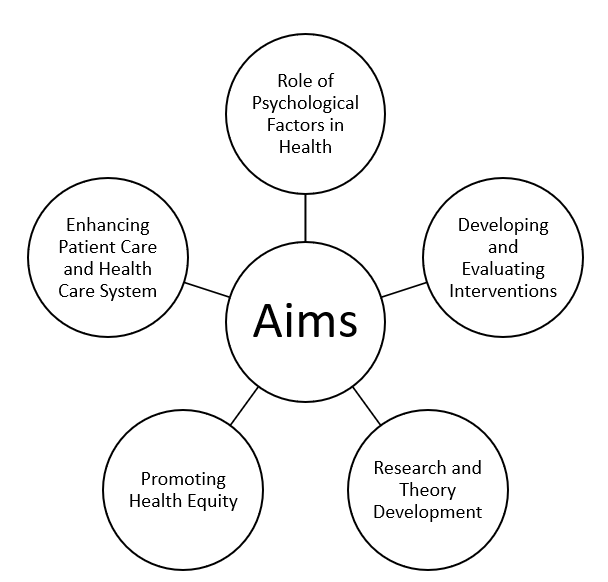
Aims of Health Psychology
Scope of Health Psychology
The scope of health psychology encompasses a wide range of topics and areas of study, reflecting its multidisciplinary nature. Key areas within the scope of health psychology include:
Health behaviours Research
Health psychologists’ study various health-related behaviours, including-
- Diet and Nutrition- Investigating the psychological factors influencing dietary choices and the effectiveness of interventions in promoting healthy eating behaviours. For example, studies have shown that motivational interviewing can enhance dietary adherence (Rubak et al., 2005).
- Physical Activity- Examining barriers to exercise and strategies to promote physical activity among different populations. Research indicates that self-determination theory can effectively enhance intrinsic motivation for physical activity (Teixeira et al., 2012).
- Substance Use- Researching the psychological aspects of addiction, including smoking, alcohol consumption, and drug use. Behavioural interventions, such as cognitive-behavioural therapy, have proven effective in reducing substance use (Monti et al., 2001).
Chronic Illness Management
Health psychology addresses the psychological aspects of living with chronic illnesses, such as-
- Diabetes- Understanding the psychological challenges faced by individuals with diabetes and developing interventions to promote self-management. Studies have shown that psychological interventions can improve glycaemic control and quality of life in diabetic patients (McGowan et al., 2015).
- Cancer- Exploring the emotional impact of cancer diagnosis and treatment, including coping strategies and support systems. Research indicates that psychological support can alleviate distress and improve quality of life for cancer patients (Faller et al., 2013).
- Cardiovascular Disease- Investigating the psychological factors related to heart health, including stress management and lifestyle changes. Studies have shown that psychological interventions can significantly reduce the risk of recurrent cardiovascular events (Blumenthal et al., 2002).
Mental Health and Well-Being
The relationship between mental health and physical health is a central focus of health psychology, including-
- Stress and Coping– Studying how stress affects health and the effectiveness of various coping strategies. Research suggests that effective stress management techniques, such as mindfulness, can improve health outcomes (Kabat-Zinn, 1990).
- Anxiety and Depression– Examining the impact of these mental health conditions on physical health and exploring interventions to improve both mental and physical well-being. Evidence indicates that integrated treatment approaches can be beneficial for individuals with comorbid conditions (Katon et al., 2007).
- Positive Psychology– Investigating how positive emotions and psychological resilience contribute to better health outcomes and longevity. Research has shown that cultivating positive emotions can enhance health and well-being (Fredrickson, 2001).
- Health Promotion and Disease Prevention
Health psychology plays a vital role in promoting health and preventing disease, focusing on-
- Health Education Programs- Developing educational initiatives to raise awareness about health risks and encourage preventive behaviours. Health literacy programs have been shown to improve individuals’ understanding of health issues and empower them to make informed decisions (Berkman et al., 2011).
- Public Health Campaigns- Collaborating with public health organizations to create campaigns that promote healthy behaviours and prevent illness. Research indicates that mass media campaigns can be effective in influencing health behaviours, such as smoking cessation and safe driving (Wakefield et al., 2010).

Scope of Health Psychology
Conclusion
Health psychology is a dynamic and interdisciplinary field that bridges the gap between psychology and medicine, focusing on the psychological, behavioural, and social factors that influence health. This field aims to understand how these factors contribute to the prevention, onset, and progression of illness and to develop interventions that promote healthier lifestyles and manage chronic conditions more effectively.
Health psychology goes beyond the traditional medical model, which emphasizes the biological aspects of disease, by incorporating psychological theories and practices into healthcare. This holistic approach acknowledges that health is not just the absence of illness but a state of complete physical, mental, and social well-being, as defined by the World Health Organization (WHO). As such, health psychologists work to understand the complex interactions between mind and body, investigating how stress, personality, social support, and coping mechanisms affect physical health outcomes.
A significant aspect of health psychology is its role in developing effective interventions aimed at behaviour change. For instance, interventions based on health psychology principles are used to promote healthier behaviours, such as smoking cessation, improved diet, and increased physical activity. These interventions are grounded in psychological theories of motivation and behaviour change, such as the Health Belief Model, the Theory of Planned behaviours, and the Transtheoretical Model of Change. By applying these models, health psychologists can design targeted interventions that motivate individuals to adopt and maintain healthier behaviours, ultimately preventing disease and enhancing quality of life.
Another crucial contribution of health psychology is in promoting health equity. Health psychologists recognize that social determinants of health, such as socioeconomic status, education, and access to healthcare, play a significant role in health outcomes. By addressing these disparities, health psychology seeks to ensure that all individuals, regardless of their background, have the opportunity to achieve optimal health. Health psychologists may work on public health campaigns, community-based interventions, or policy advocacy to address health inequities and improve access to care for underserved populations.

Important Concepts in Health Psychology
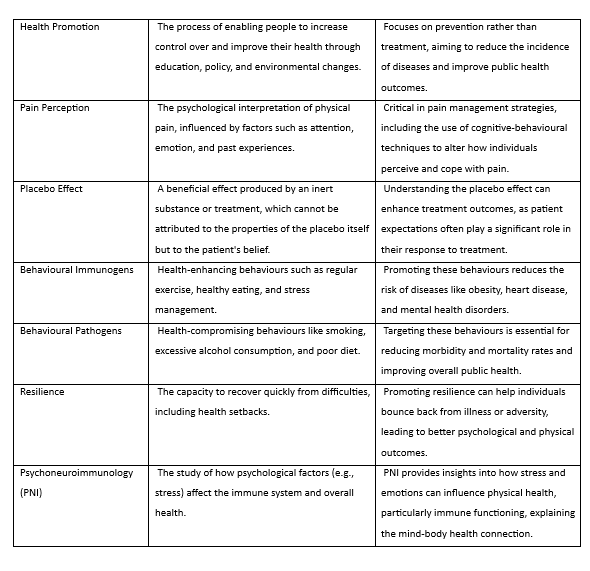
Important Concepts in Health Psychology
Moreover, health psychology plays a pivotal role in improving patient care. Health psychologists often work alongside medical professionals in clinical settings to provide psychological support to patients dealing with chronic illnesses, such as cancer, diabetes, or cardiovascular disease. By addressing the emotional and psychological aspects of illness, health psychologists help patients cope with the stress of diagnosis, treatment, and long-term management. Interventions such as cognitive-behavioural therapy (CBT), stress management techniques, and mindfulness-based interventions are commonly used to help patients improve their mental health, which in turn positively impacts their physical health outcomes.
Through research, theory, and practice, health psychologists contribute to a deeper understanding of the mind-body connection, which has practical implications for both individual and public health. Research in health psychology not only advances our understanding of the psychological processes underlying health and illness but also informs the development of evidence-based interventions that can be applied in real-world healthcare settings. For example, health psychologists may investigate how psychological factors like stress, depression, or anxiety influence the immune system or cardiovascular health, providing insights that guide the development of integrated treatment approaches.
Overall, health psychology is a vital and evolving field that plays a significant role in enhancing individual and community well-being. By integrating psychological research and clinical practice, health psychologists are uniquely positioned to address the psychological, social, and environmental factors that contribute to health and illness. Their work helps to improve patient outcomes, promote healthier lifestyles, reduce healthcare costs, and foster greater health equity across diverse populations. As healthcare systems continue to evolve and prioritize holistic approaches to wellness, the role of health psychology will remain crucial in shaping the future of health and healthcare.
References for Health Psychology
Ajzen, I. (1991). The theory of planned behaviour. Organizational behaviours and Human Decision Processes, 50(2), 179-211. https://doi.org/10.1016/0749-5978(91)90020-T
Bandura, A. (1997). Self-efficacy: The exercise of control. W.H. Freeman and Company.
Berkman, N. D., Sheridan, S. L., Donahue, K. E., Halpern, D. J., & Crotty, K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155(2), 97-107. https://doi.org/10.7326/0003-4819-155-2-201107190-00005
Blumenthal, J. A., Sherwood, A., Smith, P. J., Watkins, L., & Mabe, S. (2002). The role of psychosocial factors in outcome after coronary artery bypass graft surgery. American Psychologist, 57(11), 923-930. https://doi.org/10.1037/0003-066X.57.11.923
Champion, V. L., & Skinner, C. S. (2008). The health belief model. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behaviour and health education: Theory, research, and practice (pp. 45-65). Jossey-Bass.
Ciccarelli, S. K., & Meyer, G. E. (2006). Psychology: Concepts and connections. Pearson Education.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310-357. https://doi.org/10.1037/0033-2909.98.2.310
Donnelly, J. E., Blair, S. N., Jakicic, J. M., Manore, M. M., Rankin, J. W., & Smith, B. K. (2009). Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine & Science in Sports & Exercise, 41(2), 459-471. https://doi.org/10.1249/MSS.0b013e3181949333
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129-136. https://doi.org/10.1126/science.847460
Faller, H., Schuler, M., Richard, M., Heckl, U., Weis, J., & Küffner, R. (2013). Effects of psycho-oncologic interventions on emotional distress and quality of life in adult cancer patients: Systematic review and meta-analysis. Journal of Clinical Oncology, 31(6), 782-793. https://doi.org/10.1200/JCO.2011.40.8922
Folkman, S., & Moskowitz, J. T. (2004). Coping: Pitfalls and promise. Annual Review of Psychology, 55(1), 745-774. https://doi.org/10.1146/annurev.psych.55.090902.141456
Fredrickson, B. L. (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218-226. https://doi.org/10.1037/0003-066X.56.3.218
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delta.
Katon, W. J., Lin, E. H., & Kroenke, K. (2007). The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. General Hospital Psychiatry, 29(2), 147-155. https://doi.org/10.1016/j.genhosppsych.2006.11.005
McCormack, L. A., Treiman, K., Rupert, D., Williams-Piehota, P., Nadler, E., Arora, N. K., Lawrence, W., & Street, R. L. (2010). Measuring patient-centered communication in cancer care: A literature review and the development of a systematic approach. Social Science & Medicine, 72(7), 1085-1095. https://doi.org/10.1016/j.socscimed.2010.01.020
McGowan, P., Boddy, D., & Naji, S. (2015). Supporting people with long-term conditions: A focus on patient education and training. Patient Education and Counselling, 98(12), 1486-1491. https://doi.org/10.1016/j.pec.2015.06.014
Monti, P. M., Rohsenow, D. J., & Hutchison, K. E. (2001). Toward bridging the gap between biological, psychobiological and psychosocial models of alcohol craving. Addiction, 95(8), 1327-1340. https://doi.org/10.1046/j.1360-0443.2000.959132710.x
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustün, B. (2007). Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet, 370(9590), 851-858. https://doi.org/10.1016/S0140-6736(07)61415-9
Ogden, J. (2017). Health psychology: A textbook (5th ed.). McGraw Hill Education.
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education Monographs, 2(4), 328-335. https://doi.org/10.1177/109019817400200403
Rubak, S., Sandbæk, A., Lauritzen, T., & Christensen, B. (2005). Motivational interviewing: A systematic review and meta-analysis. British Journal of General Practice, 55(513), 305-312.
Sallis, J. F., Owen, N., & Fisher, E. B. (2006). Ecological models of health behaviour. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behaviour and health education: Theory, research, and practice (pp. 465-485). Jossey-Bass.
Satcher, D. (2006). The prevention challenge and opportunity. Health Affairs, 25(4), 1009-1011. https://doi.org/10.1377/hlthaff.25.4.1009
Stewart, M. A., Brown, J. B., Donner, A., McWhinney, I. R., Oates, J., Weston, W. W., & Jordan, J. (2000). The impact of patient-centered care on outcomes. The Journal of Family Practice, 49(9), 796-804.
Taylor, S. E. (2017). Health psychology (10th ed.). McGraw Hill Higher Education.
Teixeira, P. J., Carraça, E. V., Markland, D., Silva, M. N., & Ryan, R. M. (2012). Exercise, physical activity, and self-determination theory: A systematic review. International Journal of Behavioural Nutrition and Physical Activity, 9(1), 78. https://doi.org/10.1186/1479-5868-9-78
Wakefield, M. A., Loken, B., & Hornik, R. C. (2010). Use of mass media campaigns to change health behaviour. The Lancet, 376(9748), 1261-1271. https://doi.org/10.1016/S0140-6736(10)60809-4
Wagner, E. H., Austin, B. T., & Von Korff, M. (2001). Improving outcomes in chronic illness. Managed Care Quarterly, 9(2), 5-15.

Thank-you sir!
but how to become health psy. in india
just approach a hospital and apply