Introduction
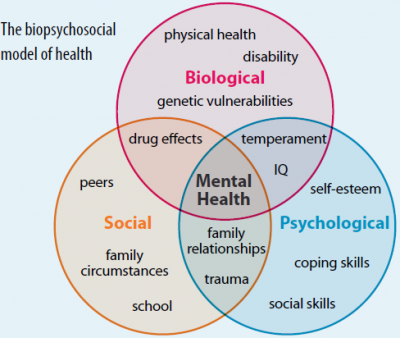
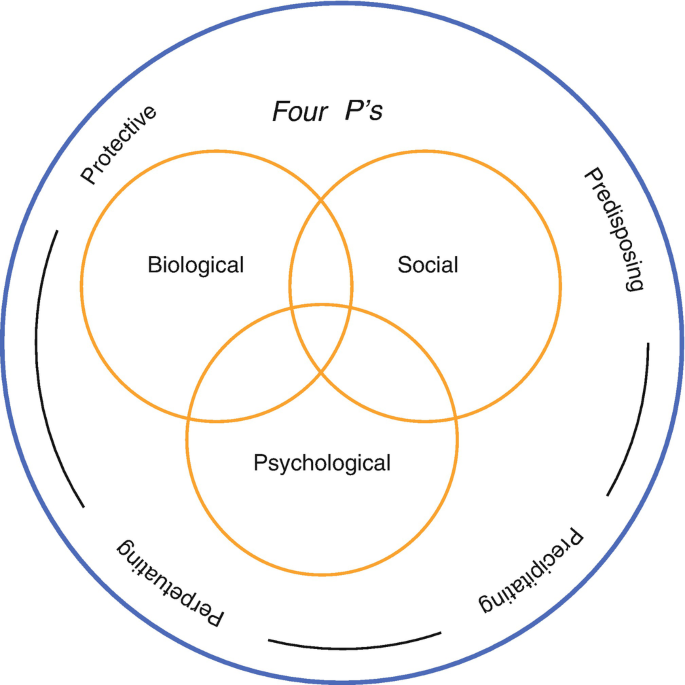
The biopsychosocial model provides a comprehensive approach to understanding health and illness. Unlike the biomedical model, which focuses solely on biological factors such as genetics, infections, and physiological dysfunctions, the BPS model integrates biological, psychological, and social influences (Engel, 1977, 1980; Kazarian & Evans, 2001).
By considering this interplay, the BPS model acknowledges that health is not just the absence of disease but a dynamic state influenced by personal behaviors, emotional well-being, and social environments. This model is widely used in healthcare and psychology to diagnose, treat, and prevent illnesses while promoting overall well-being.
Read More- Health Psychology
Biomedical Model of Health
The biomedical model of health is a traditional approach that focuses on purely biological factors in understanding disease and health. It is based on the idea that illnesses have specific biological causes (such as infections, genetic defects, or physical trauma) and can be diagnosed, treated, and cured through medical intervention.
Key Features of the Biomedical Model
Some of the key features of biomedical model include-
- Focus on Pathology- It views health as the absence of disease and considers illness as a result of abnormalities in the body’s functioning.
- Reductionist Approach- It reduces health to biological aspects, ignoring psychological and social influences.
- Diagnosis and Treatment- The model relies on medical tests, drugs, and surgeries to diagnose and treat diseases.
- Doctor-Centered- Healthcare professionals are the main decision-makers, with patients playing a passive role.
- Effective for Acute Diseases- It works well for infectious diseases, organ failures, and conditions requiring surgical intervention.
Biopsychosocial Model
The Role of Biological Factors
Biological factors refer to the physical and genetic components of health. These include-
1. Genetic Influences- Many diseases have a genetic component, meaning they can be inherited from parents. For example, conditions such as diabetes, heart disease, and certain cancers often run in families. Some genetic variations influence how a person responds to medications, making personalized medicine an important aspect of modern healthcare.
2. Physiological and Structural Functions- The body’s ability to function properly depends on the health of organs, tissues, and biochemical processes. For example-
- A malformed heart valve can impair circulation, leading to cardiovascular diseases.
- Neurotransmitter imbalances in the brain are linked to mental health conditions such as depression and schizophrenia.
The immune system also plays a critical role. A weakened immune system can make individuals more susceptible to infections, while an overactive immune system can lead to autoimmune diseases such as lupus or rheumatoid arthritis.
3. Lifestyle and Behavioral Factors- Biological health is also influenced by lifestyle choices such as diet, exercise, substance use, and sleep habits. For instance, an individual who consumes a high-fat, high-sugar diet may develop obesity and diabetes. Similarly, chronic stress can cause hormonal imbalances that increase the risk of hypertension and cardiovascular disease (Sapolsky, 2004).
Biopsychosocial Model of Evaluation and Treatment
The Role of Psychological Factors
Psychological factors involve mental and emotional processes that impact health. These include cognition, emotion, and motivation:
1. Cognition and Perception of Health- A person’s beliefs and attitudes about health influence their behaviors. Someone who believes that “smoking won’t harm me” is less likely to quit, despite knowing the risks. A person who misinterprets mild symptoms (like a headache) as a serious illness may experience health anxiety (hypochondria). Memory also plays a role in health behavior. If someone remembers a negative experience with doctors, they may avoid seeking medical care in the future.
2. Emotional States and Health Outcomes- Positive emotions, such as happiness and optimism, are linked to better immune function and faster recovery from illness. Negative emotions, such as anger, anxiety, and depression, can have adverse effects-
- Chronic stress and anxiety increase cortisol levels, which can suppress the immune system and contribute to chronic conditions like hypertension (McEwen, 1998).
- Depression is associated with reduced physical activity, poor diet, and substance abuse, which can worsen physical health (Kiecolt-Glaser et al., 2002).
3. Motivation and Health Behavior- Motivation is key in adopting and maintaining healthy behaviors. People who are intrinsically motivated to exercise (e.g., because they enjoy it) are more likely to continue than those who exercise only for external rewards. Social support can enhance motivation—for example, a smoker may quit because their child expresses concern about their health.
The Role of Social Factors
Social factors refer to interpersonal relationships, cultural norms, socioeconomic status, and societal influences that shape health behaviors and access to care.
1. Family and Peer Influence- The family environment strongly impacts health behaviors:
- Parents can model healthy habits (e.g., balanced diet, exercise) or unhealthy ones (e.g., smoking, sedentary lifestyle).
- Children exposed to healthy eating habits early in life are more likely to maintain them in adulthood.
Peer influence is particularly strong in adolescence. For example-
- Teens often begin smoking or drinking due to peer pressure (Murphy & Bennett, 2004).
- Friends who engage in physical activity together may encourage each other to maintain an active lifestyle.
2. Socioeconomic Status and Health Disparities- Income, education, and occupation impact health in several ways-
- Individuals with lower income may have limited access to nutritious food, healthcare, and exercise facilities.
- Higher education levels are associated with better health knowledge and healthier behaviors.
- Occupational hazards in low-income jobs may expose workers to harmful chemicals or physical strain.
3. Cultural and Societal Norms- Cultural beliefs influence health practices and perceptions of illness. Some cultures emphasize holistic healing, while others rely primarily on Western medicine. Societal messages (e.g., from media and advertising) can promote healthy or unhealthy behaviors. For instance, TV ads promoting junk food consumption contribute to obesity, whereas public health campaigns can encourage vaccination and smoking cessation (Harris et al., 2009).
4. Environmental Factors- The physical environment affects health behaviors-
- Communities with parks, sidewalks, and bike lanes encourage physical activity.
- Unsafe neighborhoods may deter people from exercising outdoors.
- Limited access to fresh produce in food deserts contributes to poor diet and obesity (Sallis et al., 2006).

Biopsychosocial Model for Body Dissatisfaction
Psychosomatic Medicine
Flanders Dunbar (1943) and Franz Alexander (1950) linked patterns of personality, rather than a specific conflict, to specific illnesses. They maintained that conflicts produce anxiety, which becomes unconscious and takes a physiological
toll on the body via the autonomic nervous system. The continuous physiological changes eventually produce an actual organic disturbance.
Dunbar’s and Alexander’s work helped shape the emerging field of psychosomatic medicine by offering profiles of particular disorders believed to be psychosomatic in origin, that is, caused by emotional conflicts. These disorders include hyperthyroidism, ulcers, rheumatoid arthritis, essential hypertension, neurodermatitis (a skin disorder), colitis, and bronchial asthma.
Biopsychosocial model’s assumption is that health and illness are consequences of the interplay of biological, psychological, and social factors (Keefe, 2011). According to Suls & Martin (2011,) Both macrolevel processes (like the existence of social support or the presence of depression) and microlevel processes (like cellular disorders or chemical imbalances) continually interact to influence health and illness and their course.
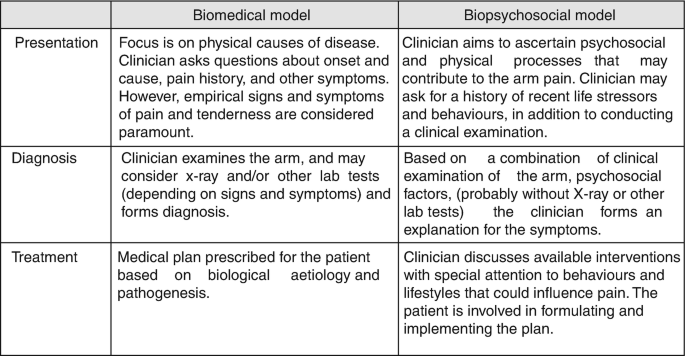
Biopsychosocial vs Biomedical Model of Health
Conclusion
The biopsychosocial model represents a paradigm shift in healthcare, recognizing that health and illness result from the interaction of biological, psychological, and social factors. This model has profound implications for medical practice, public health policies, and personal wellness strategies.
By addressing all aspects of health, individuals and healthcare providers can create more effective, personalized, and sustainable interventions to improve well-being.
References
Diehr, P., Koepsell, T., Cheadle, A., Psaty, B. M., Wagner, E., & Curry, S. (1993). Do communities differ in health behaviors? Journal of Clinical Epidemiology, 46(10), 1141-1149. https://doi.org/10.1016/0895-4356(93)90113-3
Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196(4286), 129-136. https://doi.org/10.1126/science.847460
Engel, G. L. (1980). The clinical application of the biopsychosocial model. The American Journal of Psychiatry, 137(5), 535-544. https://doi.org/10.1176/ajp.137.5.535
Harris, J. L., Bargh, J. A., & Brownell, K. D. (2009). Priming effects of television food advertising on eating behavior. Health Psychology, 28(4), 404-413. https://doi.org/10.1037/a0014399
Kazarian, S. S., & Evans, D. R. (2001). Handbook of cultural health psychology. Academic Press.
Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Psychoneuroimmunology and psychosomatic medicine: Back to the future. Psychosomatic Medicine, 64(1), 15-28. https://doi.org/10.1097/00006842-200201000-00004
McEwen, B. S. (1998). Protective and damaging effects of stress mediators. The New England Journal of Medicine, 338(3), 171-179. https://doi.org/10.1056/NEJM199801153380307
Murphy, S., & Bennett, P. (2004). Health psychology and public health. Journal of Health Psychology, 9(1), 47-65. https://doi.org/10.1177/1359105304036102
Sallis, J. F., Glanz, K., & Popham, J. (2006). Active living environments: Evidence on environmental influences on physical activity and eating behaviors. Annual Review of Public Health, 27(1), 297-322. https://doi.org/10.1146/annurev.publhealth.27.021405.102100
Sarafino, E. P. (2006). Health psychology: Biopsychosocial interactions (5th ed.). Wiley.
Sapolsky, R. M. (2004). Why zebras don’t get ulcers: The acclaimed guide to stress, stress-related diseases, and coping. Holt Paperbacks.
Story, M., Kaphingst, K. M., Robinson-O’Brien, R., & Glanz, K. (2008). Creating healthy food and eating environments: Policy and environmental approaches. Annual Review of Public Health, 29(1), 253-272. https://doi.org/10.1146/annurev.publhealth.29.020907.090926
Niwlikar, B. A. (2022, January 18). 3 Important Components of Biopsychosocial Model of Health. Careershodh. https://www.careershodh.com/what-is-biopsychosocial-model-of-health/
