Introduction to the Person in Health and Illness
Understanding health and illness requires a holistic approach that considers biological, psychological, and social influences on well-being. Health is not simply the absence of disease but a dynamic state of physical, mental, and social well-being. Similarly, illness is more than a medical condition—it encompasses how an individual experiences and responds to disease.
By examining key factors such as lifestyle, personality, and social support, we can gain a deeper insight into what determines health outcomes and how individuals can take an active role in their well-being.
Definition Of health
World Health Organisation (WHO), Health as “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity”.
Bircher (2005) defines health as “a dynamic state of well-being characterized by a physical and mental potential, which satisfies the demands of life commensurate with age, culture, and personal responsibility.”
Definition of Illness
A disease can also be defined as a state in which human capacity fluctuates and represents a deviation from biomedical standard or normal human condition.
Illness is a presentation of a medical condition in a way that limits the functional capability of an individual in the society.

Illness-Wellness Continuum
‘The Person’ is a Biopsychosocial entity with complex systems.
We know, preventative measures like better diet and personal hygiene had a major role in the fall of infectious illnesses in several countries in the late 19th century. These interventions entailed altering people’s lifestyles—their regular routines of behaviour, such cleaning, cooking, and consuming wholesome meals. Chronic diseases can also be decreased by changes in people’s lives.
Watch to discover how, are associated with the development of a disease or injury are called risk factors for that health problem. Although some risk factors are biological, like having inherited certain genes, others are behavioral.
For example, it is well known that people who smoke cigarettes face a much higher risk of developing cancer and other illnesses than nonsmokers .
Many risk factors result from the way people live or behave, such as smoking cigarettes and eating unhealthful
diets. Some behavioral risk factors-
- Heart disease associated smoking, high dietary cholesterol, obesity, and lack of exercise.
- Cancer associated smoking, high alcohol use, and diet.
- Stroke associated smoking, high dietary cholesterol, and lack of exercise.
- Chronic lung diseases associated smoking.
- Accidents (including motor vehicle)—alcohol/drug use and not using seat belts.
Read More- Biopsychosocial Approach to Health
1. Lifestyle and Illness
How influential are lifestyle factors on health?
Researchers studied two question set of people . One set asked about the health of people over the previous 12 months—for instance, whether illness had prevented them from working for a long time, forced them to cut down on other activities, or reduced their energy level.
The second set of questions asked about seven aspects of their lifestyles: sleeping, eating breakfast, eating between meals, maintaining an appropriate weight, smoking cigarettes, drinking alcohol, and getting physical activity.
Researchers found that at each age health was typically better as the number of healthful practices increased. In fact, the health of those who ‘‘reported following all seven good health practices was consistently about the same as those 30 years younger who followed few or none of these practices’’ (Belloc & Breslow, 1972, p. 419).

Common Health Practices and Health Care
Why don’t people do what’s good for them?
There’s no simple answer to that question—there are many reasons. These include-
- Immediate Pleasure- Less healthful behaviors often bring immediate pleasure, as when the person has a ‘‘goodtasting’’ cigarette or ice cream. Its Long-range negative consequences seem remote, both in time and in likelihood.
- Social pressures- This includes to engage in unhealthful behavior, as when an adolescent begins to use cigarettes, alcohol, or drugs.
- Addiction- Some behaviors can become very strong habits, perhaps involving a physical addiction or psychological dependency.- cigarettes, alcohol, or drugs.
- Ignorant- There are situations when people are merely ignorant of the risks involved or how to alter their conduct. These individuals require knowledge on how to safeguard their health.
Keep in mind that pleasurable lifestyles can benefit health: some evidence suggests that engaging in enjoyable activities, such as vacationing or attending concerts, may lead to better health (Bygren et al., 2009; Pressman et al., 2009).
2. Personality and Illness
Researchers have found evidence linking personality (Consistent pattern of thinking, feeling and behaving) traits and health. For example, people whose personalities include-
- Low levels of conscientiousness measured in childhood or adulthood are more likely to die at earlier ages, such as from cardiovascular diseases, than individuals high in conscientiousness (Kern & Friedman, 2008; Terracciano et al., 2008).
- High levels of positive emotions, such as happiness or enthusiasm, tend to live longer than individuals with
low levels of these emotions (Chida & Steptoe, 2008; Xu & Roberts, 2010). - High levels of anxiety, depression, hostility, or pessimism are at risk for dying early and developing a variety of illnesses, particularly heart disease (Grossardt et al., 2009; Smith & Gallo, 2001).
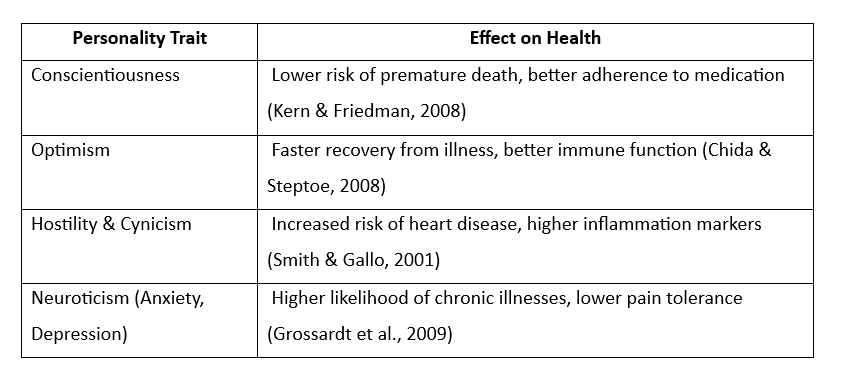
Personality and Health Consequences
Personality and illness is two-way street- illness can affect one’s personality, too (Cohen & Rodriguez, 1995).
Health psychology suggests that “The Person” should be seen as complex systems and that illness is caused by a multitude of factors and not by a single causal factor. Health psychology therefore attempts to move away from a
simple linear model of health and claims that illness can be caused by a combination of biological (e.g. a virus), psychological (e.g. behaviours, beliefs) and social (e.g. employment) factors.
According to health psychology, “the whole person” should be treated, not just the physical changes that have taken place. This can take the form of behaviour change, encouraging changes in beliefs and coping strategies and compliance with medical recommendations.
Illness is regarded as a result of a combination of factors, the individual is no longer simply seen as a passive victim. For example, the recognition of a role for behaviour in the cause of illness means that the individual may be held responsible for their health and illness.
Who is responsible for treatment? Because the whole person is treated, not just their physical illness, the patient is therefore in part responsible for their treatment. This may take the form of responsibility to take medication, responsibility to change beliefs and behaviour. They are not seen as a victim.
Biopsychosocial model’s assumption is that the person’s health and illness are consequences of the interplay of biological, psychological, and social factors (Keefe, 2011).
According to Suls & Martin (2011,) Both macrolevel processes (like the existence of social support or the presence of depression) and microlevel processes (like cellular disorders or chemical imbalances) continually interact to influence health and illness and their course.
So, when a person is healthy or ill, it will affect every domain of that persons life, His/her private and public life. It will affect his/her biological, psychological, social, political, environmental etc. Healthy person will excel in all of these domains where as Ill person will limit in every capacity of that person.
References
Ogden, J. (2017). Health psychology: A textbook (4th ed.).McGraw Hill Education.
Sarafino, E. P. and Smith, T.W. (2012). Health Psychology – Bio psychosocial Interaction (7th ed). Wiley India (Ed)
Taylor, Shelley E. (2018). Health Psychology (10th ed). McGraw Hill Higher Education. Indian Edition
Larson J. S. The conceptualization of health. Medical Care Research and Review. 1999;56(2):123–136
Subscribe to Careershodh
Get the latest updates and insights.
Join 16,504 other subscribers!
Niwlikar, B. A. (2022, November 27). The Person in Health and Illness and Its 2 Important Implications. Careershodh. https://www.careershodh.com/the-person-in-health-and-illness/
