Introduction to Neurotransmitters and nervous system
Neurotransmitters are chemical messengers in the nervous system, essential for transmitting signals between neurons and regulating bodily functions & behaviors. These neurotransmitters, including dopamine, serotonin, norepinephrine, and acetylcholine, influence key processes such as mood, memory, motor control, and attention. A balanced neurotransmitter system ensures proper physiological and psychological behavior.
Imbalances in neurotransmitter activity can contribute to various diseases and disorders (Teleanu, et.al 2022). For example, Parkinson’s disease is linked to dopamine deficiency, while depression and anxiety often involve serotonin imbalances. Understanding these systems is crucial for developing effective treatments for these conditions.
Definition of Neurotransmitter
According to American Psychological Association (APA), “any of a large number of chemicals that can be released by neurons to mediate transmission of nerve signals across the junctions (synapse) between neurons.”
Neurotransmitters are molecules that amplify, transmit, and convert signals in cells, having an essential role in information transmission throughout the nervous system (Teleanu, et.al 2022).
Read about Role of Neurotransmitters in Synaptic Transmission
Behavioral Pharmacology
Biopsychologists often rely on pharmacological methods to study the relationship between neurotransmitters and behavior. These methods involve administering drugs to human or nonhuman subjects, targeting specific neurotransmitter systems, and then observing how these drugs affect behavior.
Drugs can have two primary effects on synaptic transmission: they can either facilitate or inhibit it.
- Agonists are substances that enhance or mimic the action of a particular neurotransmitter, boosting its effect on the nervous system.
- On the other hand, antagonists block or dampen the action of a neurotransmitter, preventing its normal effect.
By using agonists and antagonists, researchers can gain valuable insights into how neurotransmitters influence behavior and contribute to various psychological and neurological conditions.
Mechanism of Drug Action
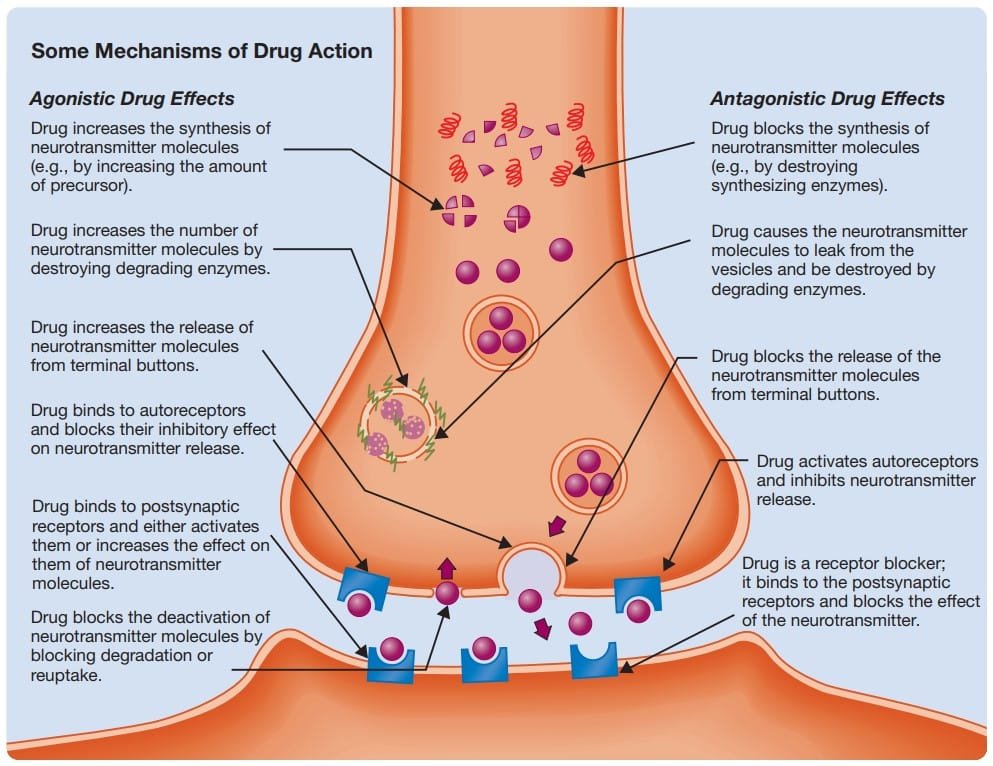
Mechanism of Drug Action
Types of Neurotransmitters
There are two types of neurotransmitters (NT) : Small Molecule NTs and Large Molecule NTs
Small Molecule Neurotransmitters
1. Amino Acid : Amino acids, the molecular building blocks of proteins, are prevalent neurotransmitters in fast-acting synapses within the central nervous system.
- Key NTs: Glutamate, aspartate, glycine, and gamma-aminobutyric acid (GABA).
- Glutamate: The most common excitatory neurotransmitter in the mammalian CNS.
- GABA: The primary inhibitory neurotransmitter, though it exhibits excitatory effects at certain synapses (Valeeva, Valiullina, & Khazipov, 2013; Watanabe, Fukuda, & Nabekura, 2014). GABA is derived from glutamate through structural modification.
2. Monoamine : Monoamines are small-molecule neurotransmitters synthesized from single amino acids. Their effects are more diffuse compared to amino acids.
- Key neurotransmitters: Dopamine, epinephrine, norepinephrine, and serotonin.
- Subdivisions:
- Catecholamines: Dopamine, norepinephrine, and epinephrine, synthesized from tyrosine via intermediates like L-dopa.
- Indolamines: Serotonin (5-HT), synthesized from tryptophan (Watanabe et al., 2014).
- Location: Primarily found in small groups of neurons in the brainstem with branched axons for widespread release
- Subdivisions:
3. Acetylcholine : A unique small-molecule neurotransmitter formed by combining an acetyl group with choline.
- Functions:
- Active at neuromuscular junctions, autonomic nervous system synapses, and in parts of the central nervous system.
- Degraded by acetylcholinesterase in synapses.
- Neurons releasing acetylcholine are termed cholinergic.
4. Unconventional Neurotransmitters : These NTs operate in atypical ways:
- Soluble-Gas: Include nitric oxide and carbon monoxide.
- Characteristics: Produced in neural cytoplasm, diffuse through membranes, act on second messengers, and are short-lived (Iremonger, Wamsteeker Cusulin, & Bains, 2013).
- Function: Involved in retrograde transmission to regulate presynaptic neuron activity.
- Endocannabinoids: Include anandamide, resembling THC (the psychoactive component of marijuana).
- Characteristics: Synthesized from fatty compounds, released from dendrites or cell bodies, and inhibit presynaptic transmission (Katona & Freund, 2012)
Large Molecule Neurotransmitter
Neuropeptides : They Composed of amino acid sequences, neuropeptides perform diverse functions. Approximately 100 have been identified and categorized as follows:
- Pituitary Peptides: First identified as pituitary hormones.
- Hypothalamic Peptides: First identified as hypothalamic hormones.
- Brain–Gut Peptides: Initially discovered in the gut.
- Opioid Peptides: Structurally similar to opium’s active ingredients.
- Miscellaneous Peptides: Neuropeptides not fitting into the above categories.
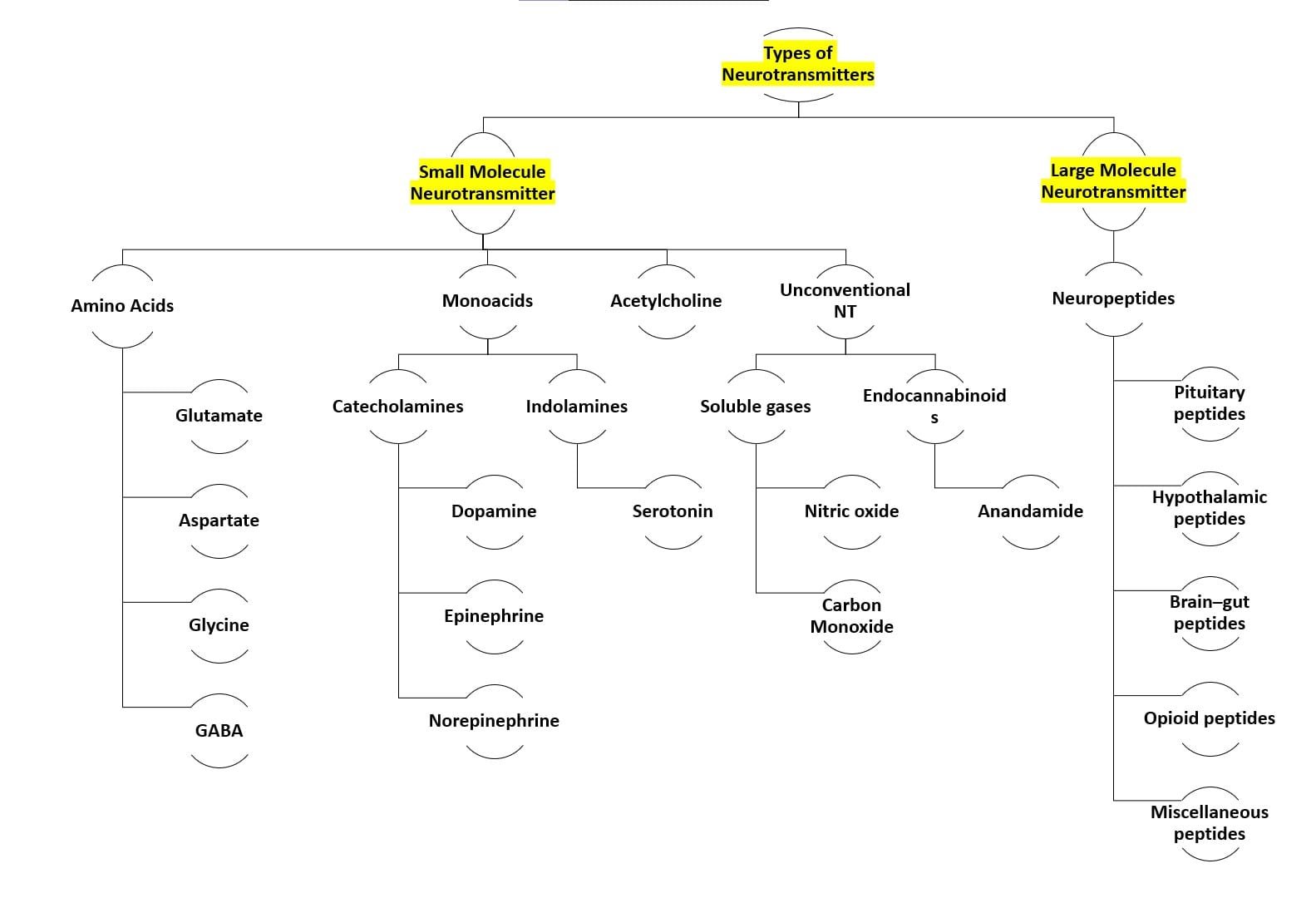
Types of neurotransmitters
Neurotransmitters in Peripheral Nervous System
Effect of neurotransmitter on Somatic Nervous System
The Somatic Nervous System (SNS) is responsible for controlling voluntary movements of the body’s skeletal muscles, which include those in the limbs, face, trunk, and other body parts. It is influenced significantly by neurotransmitters, particularly acetylcholine (ACh), which serves as the primary neurotransmitter at neuromuscular junctions.
1. Acetylcholine and Motor Neurons
Motor neurons in the brain and spinal cord transmit signals to skeletal muscles, enabling movement. These neurons are called cholinergic neurons because acetylcholine (ACh) is their primary neurotransmitter. ACh is excitatory at the neuromuscular junction (the synapse between the motor neuron and the muscle fibre), meaning that it facilitates muscle contraction. When ACh is released into the synaptic cleft, it binds to receptors on the muscle fibre, triggering a series of events that lead to muscle contraction.
2. Nicotinic Acetylcholine Receptor (nAChr)
The nicotinic acetylcholine receptor (nAChr) is a specific ionotropic receptor located on muscle fibers. When acetylcholine (ACh) binds to this receptor, it opens an ion channel that allows sodium (Na⁺) to enter the muscle cell and potassium (K⁺) to exit, which causes the muscle cell to become depolarized. This depolarization is a key step in initiating muscle contraction. The nicotine molecule, found in tobacco, has a molecular structure similar to that of acetylcholine, enabling it to bind to the nAChr and activate it in the same way as ACh. This explains why nicotine acts as a mimic for acetylcholine.
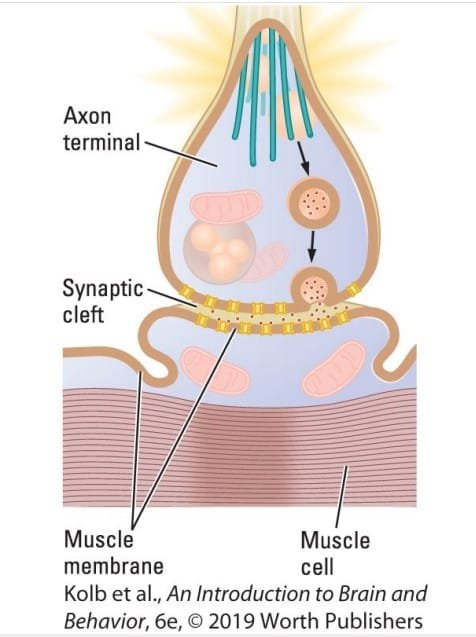
Nicotinic ACh Receptor
3. Role of Neuropeptides and Other Neurotransmitters
While acetylcholine is the primary neurotransmitter in the SNS, other molecules, such as the calcitonin gene-related peptide (CGRP), also contribute to muscle function. CGRP is released alongside acetylcholine at cholinergic axon terminals. Once released, CGRP acts on CGRP metabotropic receptors on the muscle to increase the force of muscle contractions, thereby enhancing muscle performance.
4. Clinical Implications
Dysfunctions in neurotransmission at the neuromuscular junction, such as myasthenia gravis (a condition where ACh receptors are blocked or destroyed), can impair muscle function. Similarly, the effects of nicotine on nAChr receptors can alter normal neuromuscular communication, which is why nicotine and other substances that act on these receptors can influence muscle activity and overall motor control.
Cholinergic Agonists and Antagonists
Drugs like curare block nicotinic receptors, leading to paralysis by preventing muscle contraction. This mechanism is utilized during surgeries to inhibit involuntary muscle movements (Changeux, 2013; Papke, 2014).
Effect of neurotransmitter on Autonomous Nervous System
The Autonomic Nervous System (ANS) consists of two complementary divisions: the sympathetic and parasympathetic systems. These divisions maintain the body’s internal environment by regulating involuntary physiological functions like heart rate, digestion, and respiration.
Sympathetic Division
It Activates the “fight-or-flight” response, preparing the body for action. It increases heart rate and blood pressure, decreases digestive activity and dilates pupils & airways.
Role of Neurotransmitter in fight/ flight Response: Norepinephrine (NE) is the primary neurotransmitter. It binds to receptors on various organs:
- Excitatory effects: Increases heart rate by binding to β-adrenergic receptors.
- Inhibitory effects: Reduces digestive activity by acting on α-adrenergic receptors in the gastrointestinal tract.
Parasympathetic Division
It activates the “rest-and-digest” response, calming the body. It decreases heart rate, stimulates digestion and glandular activity and constricts pupils & airways.
Role of Neurotransmitter: Acetylcholine (ACh) is the primary neurotransmitter, acting on muscarinic receptors:
- Inhibitory effects: Slows heart rate by binding to M2 receptors.
- Excitatory effects: Enhances digestive activity by acting on M3 receptors

Neurotransmitter affecting ANS
Integrated Regulation
The interplay of norepinephrine and acetylcholine in the sympathetic and parasympathetic divisions creates a dynamic balance. This balance adjusts the body’s internal state according to situational demands:
- In stressful situations, the sympathetic system dominates to prioritize energy use.
- In relaxed states, the parasympathetic system takes over to conserve energy and promote restoration.
This reciprocal regulation exemplifies how neurotransmitter activity can both excite and inhibit functions depending on the specific receptors and organs involved.
Effect of neurotransmitter on Central Nervous System
Each of four small-molecule transmitters participates in its own neural activating system—the cholinergic, dopaminergic, noradrenergic and serotonergic systems. Each CNS activating system is associated with numerous behaviors. Associations among
activating systems, behavior, and brain disorders are far less certain. All these relations are subjects of ongoing research.
A. Cholinergic System
The cholinergic system, a neural network that utilizes acetylcholine (ACh) as its primary neurotransmitter, is integral to various cognitive and physiological processes.
🟢 Anatomy and Neurochemical Basis
Acetylcholine’s action in the brain is regulated by the enzyme acetylcholinesterase (AChE), which breaks down ACh at synapses to terminate its activity. Regions with high AChE concentrations, such as the basal ganglia and cortex, indicate dense cholinergic activity. These areas often receive input from cholinergic nuclei located in the brainstem.
🟢 Functional Roles of the Cholinergic System
The cholinergic system is crucial for maintaining waking behavior, regulating typical wakeful states, and producing specific EEG activity patterns. Beyond arousal, it is also deeply involved in attention and memory processes. Cholinergic neurons facilitate the ability to focus and encode memories, which are essential for daily cognitive functioning.
🟢 Cholinergic Dysfunction in Alzheimer’s Disease
In Alzheimer’s disease, the loss of cholinergic neurons is a hallmark feature. This degenerative disorder typically begins with minor forgetfulness, which progresses to severe memory impairment and generalized dementia. Autopsies of Alzheimer’s patients reveal significant damage to cholinergic neurons, particularly in regions associated with memory and cognition.
This loss of cholinergic function often accompanies extensive degeneration in the neocortex and other brain regions, suggesting a complex interplay between cortical damage and cholinergic deficits. It remains unclear whether cortical degeneration causes cholinergic neuron loss or vice versa.
🟢 Treatment Targeting the Cholinergic System
- Acetylcholinesterase Inhibitors (AChEIs): Drugs such as donepezil increase ACh availability by inhibiting its breakdown.
- Nicotinic Receptor Modulation: Enhancing the number or sensitivity of nicotinic ACh receptors may improve cognitive symptoms.
- Dietary Interventions: The role of diet in maintaining acetylcholine synthesis is under investigation, with the potential for dietary strategies to support cholinergic function.
- Cell Death Prevention: Emerging therapies aim to prevent neuronal degeneration, thereby slowing disease progression.
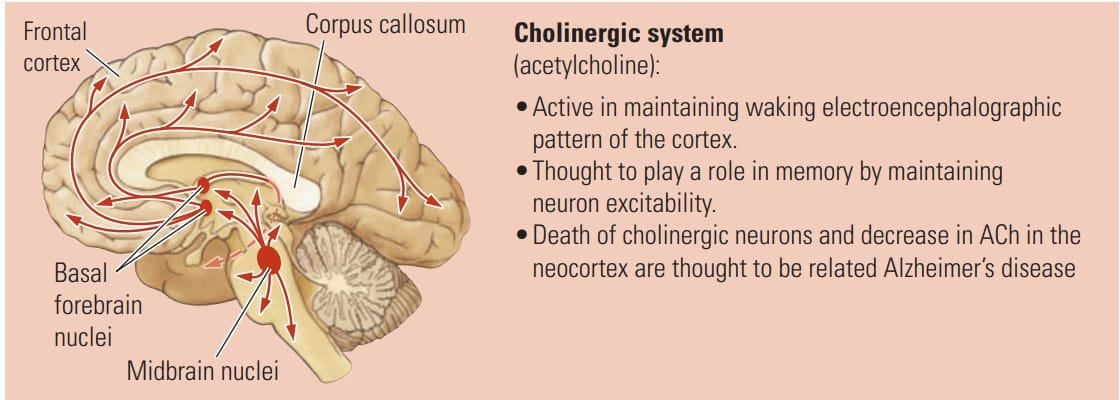
Cholinergic System
B. Dopaminergic System
The dopaminergic system plays a crucial role in regulating movement, motivation, reward, and several other key behaviors. As the name suggest, the primary neurotransmitter is Dopamine. Dysfunction in this system is linked to severe neurological and psychiatric disorders, including Parkinson’s disease, addiction, and schizophrenia.
🟢 Pathways of the Dopaminergic System : It operates through two major pathways:
- Nigrostriatal Dopaminergic System: This pathway is essential for coordinating movement. Dopamine neurons originating in the substantia nigra project to the striatum, enabling smooth motor function.
- In Parkinson’s disease, the loss of dopamine neurons in the substantia nigra leads to extreme muscular rigidity, where opposing muscles contract simultaneously, restricting movement.
- Rhythmic tremors of the limbs, often observed in Parkinson’s patients, are thought to result from the release of formerly inhibited motor signals.
- Though the exact causes of Parkinson’s disease remain uncertain, exposure to certain neurotoxic drugs can selectively damage dopamine neurons, as noted in the case study “The Frozen Addict.”
- Mesolimbic Dopaminergic System: This pathway is critical for regulating motivation, reward, and impulse control.
- Dopamine activity in this system underpins addictive behaviors, including compulsive consumption of food, drugs, and engagement in other rewarding activities. Environmental stimuli, when associated with dopamine release, become highly attractive and rewarding, reinforcing addictive behaviors.
- Interestingly, Parkinson’s patients treated with dopamine receptor agonists may exhibit impulsive behaviors such as pathological gambling, hypersexuality, or compulsive shopping (Moore et al., 2014).
🟢 Dopamine and Psychiatric Disorders
Excessive activity in the mesolimbic dopaminergic system has been implicated in schizophrenia, a complex psychiatric disorder.
- Schizophrenia manifests with a range of symptoms, including delusions, hallucinations, disorganized speech, blunted emotional responses, and agitation or immobility.
- Dopamine dysregulation is believed to contribute to the positive symptoms of schizophrenia, such as hallucinations and delusions, while other neurotransmitter systems may underlie the negative symptoms, such as emotional flattening.
- Schizophrenia is highly prevalent, affecting approximately 1 in 100 people globally, and remains one of the most debilitating mental health conditions.
🟢 Clinical Implications : Understanding the dopaminergic system provides critical insights into both neurological and psychiatric conditions.
- Parkinson’s Disease: Dopamine replacement therapies, such as levodopa, aim to restore dopamine levels in the nigrostriatal pathway, improving motor symptoms.
- Addiction: Research into dopamine modulation may yield new interventions for treating substance use disorders and compulsive behaviors.
- Schizophrenia: Dopamine receptor antagonists, such as antipsychotic medications, target excessive dopaminergic activity to mitigate symptoms. However, the complexity of the disorder necessitates a broader therapeutic approach.
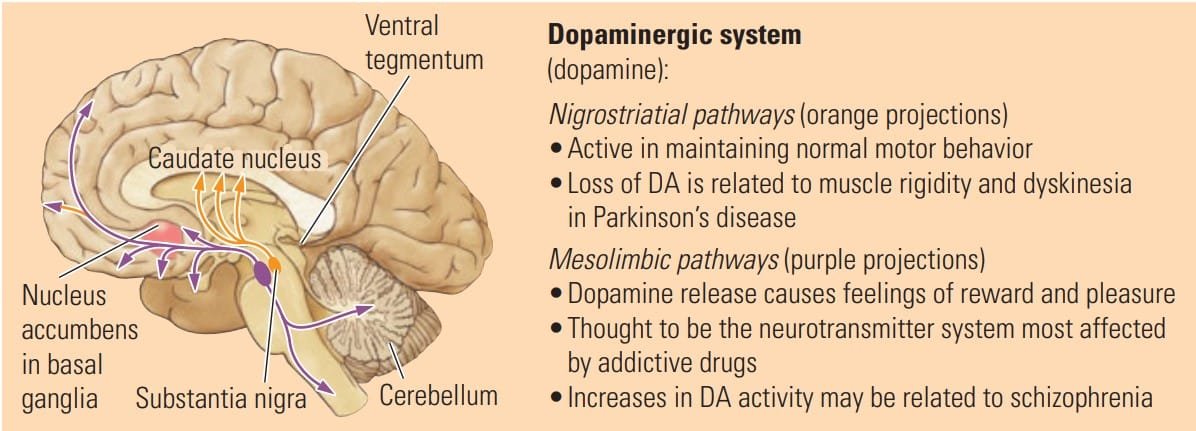
Dopaminergic System
C. Noradrenergic System
The noradrenergic system, driven by neurons that use norepinephrine (noradrenaline) as their transmitter, plays a critical role in learning, brain development, and emotional regulation. Dysfunction in this system is linked to mood disorders and behavioral conditions, highlighting its significance in maintaining mental health.
🟢 Functions of the Noradrenergic System
- Learning and Neural Plasticity: Norepinephrine stimulates neurons to undergo structural changes, thereby facilitating learning and memory formation. It may also contribute to healthy brain development, helping to establish neural networks necessary for cognitive and motor functions.
- Motor Organization: This neurotransmitter supports the organization of movements, ensuring coordinated and purposeful motor actions.
🟢 Noradrenergic System and Emotional Regulation : The noradrenergic system is intricately linked to emotional behaviors and mood disorders.
- Major Depression: Decreased activity of noradrenergic neurons is associated with symptoms of major depression, including prolonged feelings of worthlessness, disrupted eating and sleeping habits, and slowed behavior. These disruptions suggest that norepinephrine plays a pivotal role in regulating mood and energy levels.
- Mania: Conversely, increased activity in the noradrenergic system has been linked to mania, a state characterized by excessive excitability, impulsivity, and heightened energy levels.
- ADHD and Hyperactivity: Decreased norepinephrine activity is also implicated in conditions like attention-deficit/hyperactivity disorder (ADHD) and hyperactivity, suggesting its role in maintaining attention and behavioral control.
🟢 Clinical Implications
- Antidepressant Medications: Drugs targeting norepinephrine levels, such as selective norepinephrine reuptake inhibitors (SNRIs), are commonly prescribed for mood disorders.
- ADHD Treatments: Norepinephrine-modulating medications, such as atomoxetine, are used to improve attention and reduce hyperactivity.
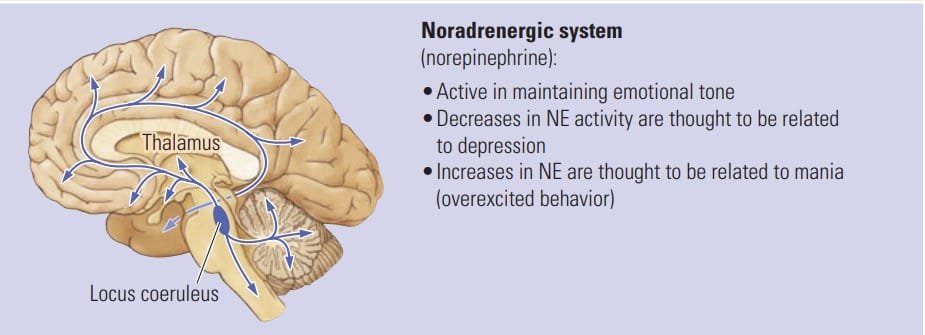
Noradrenergic System
D. Serotonergic system
The serotonergic system, driven by serotonin (5-HT) neurons, plays a critical role in regulating wakefulness, mood, learning, and behavior. Dysfunction in this system is associated with various psychiatric and neurological conditions, underscoring its significance in maintaining mental and physiological balance.
🟢 Functions of the Serotonergic System
- Wakefulness and Brain Activity: The serotonergic system helps maintain a waking EEG in the forebrain during movement, promoting wakefulness in conjunction with the cholinergic system.
- Role in Learning: Similar to norepinephrine, serotonin contributes to learning processes, enhancing cognitive functioning.
🟢 Serotonergic System and Mental Health Disorders
- Depression: Decreased serotonergic activity is linked to some forms of depression. Antidepressant drugs, such as selective serotonin reuptake inhibitors (SSRIs), work by modulating serotonin levels to alleviate depressive symptoms. This dual role of norepinephrine and serotonin in depression suggests the existence of different subtypes of depression, each tied to specific neurotransmitter imbalances.
- Schizophrenia: Increased serotonergic activity has been implicated in certain symptoms of schizophrenia, hinting at possible subtypes of schizophrenia related to serotonin dysregulation.
- Obsessive-Compulsive Disorder (OCD): Reduced serotonin activity is associated with OCD, a condition characterized by repetitive thoughts (obsessions) and behaviors (compulsions). Serotonin-targeted treatments often alleviate OCD symptoms, emphasizing its role in the disorder.
- Sleep and Respiratory Disorders: Abnormalities in serotonergic nuclei have been linked to sleep apnea and sudden infant death syndrome (SIDS). These findings highlight serotonin’s role in regulating vital autonomic functions.
🟢 Clinical Implications
- SSRIs and Other Antidepressants: These medications are crucial for treating depression and anxiety disorders by enhancing serotonin activity.
- Targeted OCD Therapies: Treatments focusing on serotonergic modulation show promise in alleviating symptoms of obsessive-compulsive behaviors.
- Schizophrenia Research: Exploring the role of serotonin in schizophrenia can guide the development of therapies tailored to its specific subtypes.

Serotonergic System
Conclusion
Neurotransmitters are fundamental to the functioning of the nervous system, directly influencing behavior, emotions, and cognitive processes. Their delicate balance ensures optimal physiological performance, while disruptions in their activity are often at the core of many neurological and psychological disorders. Advancing our understanding of neurotransmitter systems opens the door to better diagnostic methods and more targeted treatments for conditions like Parkinson’s disease, depression, and schizophrenia. Continued research in this field holds the potential to significantly improve mental health and overall well-being.
References
- Kalat, J. W. (2019). Biological psychology. Cengage.
- Kolb, B., & Whishaw, I. Q. (2019). An introduction to brain and behavior.
- Pinel, J. (2018). Biopsychology 10th Edition. Pearson
- Teleanu, R. I., Niculescu, A. G., Roza, E., Vladâcenco, O., Grumezescu, A. M., & Teleanu, D. M. (2022). Neurotransmitters-Key Factors in Neurological and Neurodegenerative Disorders of the Central Nervous System. International journal of molecular sciences, 23(11), 5954. https://doi.org/10.3390/ijms23115954
Subscribe to Careershodh
Get the latest updates and insights.
Join 16,604 other subscribers!
Niwlikar, B. A. (2025, January 21). Importance of Neurotransmitters in functioning of Nervous system. Careershodh. https://www.careershodh.com/neurotransmitters-in-nervous-system/
