CHANGING HEALTH HABITS
Some of the ways to change bad habits and develop health habits include-
- Educational Appeals- Educational appeals make the assumption that people will change their health habits if they have good information about their habits. Early and continuing efforts to change health habits have focused heavily on education and changing attitude.
- Fear Appeals- Attitudinal approaches to changing health habits often make use of fear appeals. This approach assumes that if people are afraid that a particular habit is hurting their health, they will change their behavior to reduce their fear.
- Message Framing- A health message can be phrased in positive or negative terms. For example, a reminder card to get a flu immunization can stress the benefits of being immunized or stress the discomfort of the flu itself (Gallagher, Updegraff, Rothman, & Sims, 2011). Messages that emphasize problems seem to work better for behaviors that have uncertain outcomes, for health behaviors that needs practice only once. Such as vaccinations and for issues about which people are fearful. Messages that stress benefits are more persuasive for behaviors with certain outcomes.
People who have a promotion or approach orientation that emphasizes maximizing opportunities are more influenced by messages phrased in terms of benefits (“calcium will keep your bones healthy”). Whereas, people who have a prevention or avoidance orientation that emphasizes minimizing risks are more influenced by messages that stress the risks of not performing a health behavior (“low calcium intake will increase bone loss”) (Mann, Sherman, & Updegraff , 2005). On the whole, promotion-oriented messages may be somewhat more successful in getting people to initiate behavior change, and prevention messages may be more helpful in getting them to maintain behaviour change over time (Fuglestad, Rothman, & Jeff ery, 2008).
Theories for Changing Health Habits
The theories of changing bad habits and developing healthy habits include-
1. The Health Belief Model
The Health Belief Model (HBM) was developed in the 1950’s by social psychologists Hochbaum, Rosenstock and others. An early influential attitude theory of why people practice health behaviours is the health belief model (Hochbaum, 1958; Rosenstock, 1966). According to this model, whether a person practices a health behaviour depends on two factors: whether the person perceives a personal health threat, and whether the person believes that a particular health practice will be effective in reducing that threat.

Health Belief Model
Three factors influence the perception of a personal health threat:
- General health values, which include interest in and concern about health;
- Specific beliefs about personal vulnerability to a particular disorder (Dillard, Ferrer, Ubel, & Fagerlin, 2012); and
- Beliefs about the consequences of the disorder, such as whether they are serious. Whether a person believes a health measure will reduce threat has two subcomponents: whether the person thinks the health practice will be effective, and whether the cost of undertaking that measure exceeds its benefits.
2. The Theory of Planned Behaviour
Health beliefs go some distance in predicting when people will change their health habits. A theory that attempts to link health beliefs directly to behaviour is Ajzen’s theory of planned behaviour (Ajzen & Madden, 1986; Fishbein & Ajzen, 1975). According to this theory, a health behaviour is the direct result of a behavioural intention.
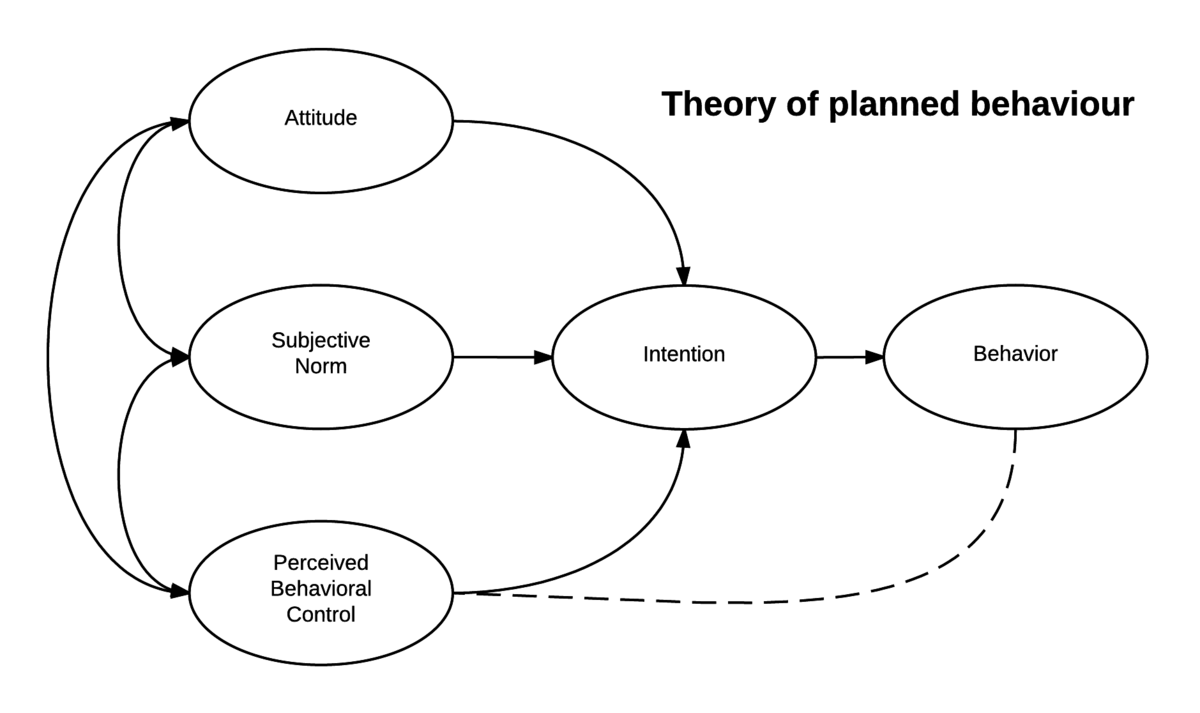
Theory of Planned Behavior
However, behavioral intentions are of three components:
- Attitudes toward the specific action,
- Subjective norms regarding the action, and
- Perceived behavioral control.
Moreover, attitudes toward the action center on the likely outcomes of the action and evaluations of those outcomes.
Read More- Self Determination Theory
3. Self-Determination Theory
Self-determination theory (SDT), a theory that also guides health behaviour modification, builds on the idea that people are actively motivated to pursue their goals (Deci & Ryan, 1985; Ryan & Deci, 2000). The theory targets two important components as fundamental to behaviour change, namely autonomous motivation and perceived competence. People are autonomously motivated when they experience free will and choice when making decisions. Similarly, competence refers to the belief that one is capable of making the health behaviour change.
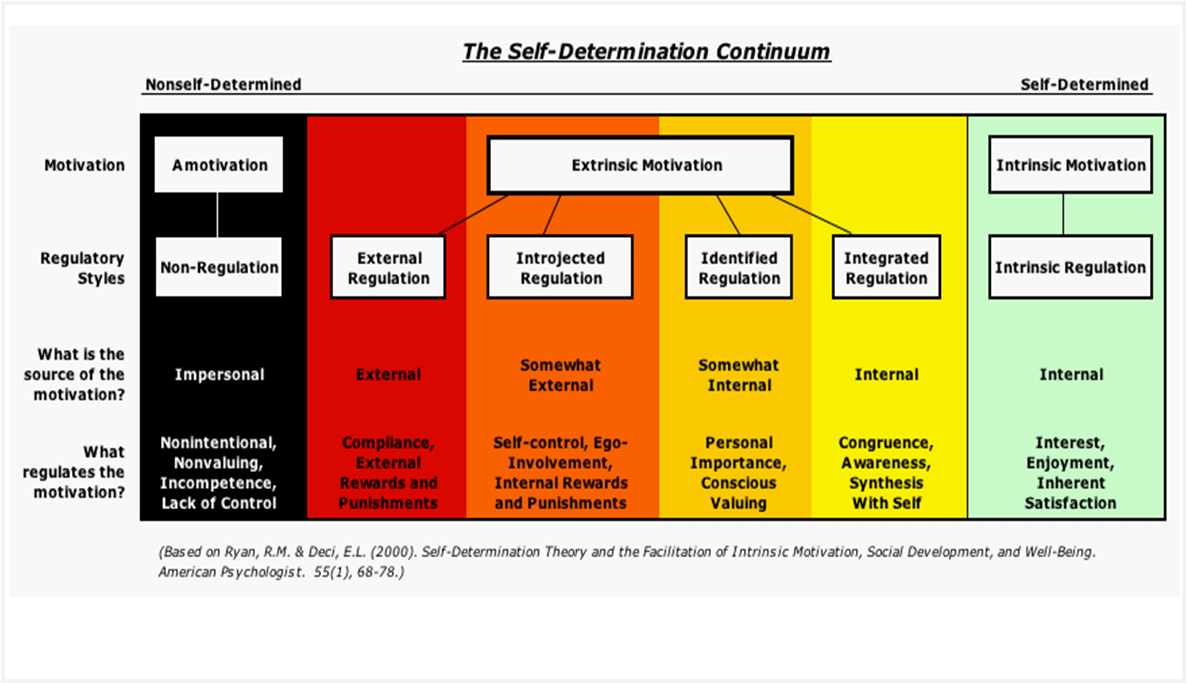
Self Determination Theory
Cognitive Behavioural Approaches to Behaviour Change
Some of the cognitive behavioural approaches include-
- Cognitive-Behaviour Therapy (CBT)- Cognitive-behaviour approaches to health habit modification focus on the target behaviour itself, the conditions that elicit and maintain it, and the factors that reinforce it (Dobson, 2010). The most effective approach to health habit modification often comes from cognitive behaviour therapy (CBT). CBT interventions use several complementary methods to intervene in the modification of a target problem and its context. However, CBT may be implemented individually, through therapy in a group setting, or even on the Internet. It is a versatile as well as effective way of intervening to modify poor health habits.
- Self-Monitoring- Many programs of cognitive-behavioural modification use self-monitoring as the first step toward behaviour change. The rationale is that a person must understand the dimensions of the poor health habit before change can begin. Self-monitoring assesses the frequency of a target behaviour and the antecedents and consequences of that behaviour.
- Stimulus Control- Once the circumstances surrounding the target behavior are well understood, the factors in the environment that maintain poor health habits such as smoking, drinking, and overeating, can be modified. Stimulus-control interventions involve ridding the environment of discriminative stimuli. That stimuli evokes the problem behavior, and creating new discriminative stimuli, signaling that a new response will be reinforced.
- The Self-Control of Behavior- Cognitive-behavior therapy focuses heavily on the beliefs that people hold about their health habits. People often generate internal monologues that interfere with their ability to change their behavior. For example, a person who wishes to give up smoking may derail the quitting process by generating self-doubts (.“I will never be able to give up smoking”). Unless these internal monologues are modified, the person will be unlikely to change a health habit and maintain that change over time.
- Self-Reinforcement- Self-reinforcement involves systematically rewarding oneself to increase or decrease the occurrence of a target behavior. In addition positive self-reward involves rewarding oneself with something desirable after successful modification of a target behavior. Such as going to a movie following successful weight loss. Negative self-reward involves removing an aversive factor in the environment after successful modification of the target behavior. An example of negative self-reward is taking the Miss Piggy poster off the refrigerator once she achieves the regular controlled eating.
- Classical Conditioning- Classical conditioning is the pairing of an unconditioned reflex with a new stimulus, producing a conditioned reflex. It was one of the first methods for health behavior change.
- Operant Conditioning- In contrast to classical conditioning, which pairs an automatic response with a new stimulus, operant conditioning pairs a voluntary behavior with systematic consequences. The key to operant conditioning is reinforcement. When a person performs a behavior and that behavior is followed by positive reinforcement, the behaviour is more likely to occur again. Similarly, if an individual performs a behavior and reinforcement is withdrawn or the behaviour is punished, the behaviour is less likely to be repeated. Over time, these contingencies build up those behaviours paired with positive reinforcement. Whereas punished or not rewarded behavior decline.
- Modeling- Modeling is learning that occurs from witnessing another person perform a behaviour (Bandura, 1969). Observation and subsequent modeling can be effective approaches to changing health habits. For example, in one study high school students who observed others donating blood were more likely to do so themselves (Sarason, Sarason, Pierce, Shearin, & Sayers, 1991).
- Behavioral Assignments- A technique for increasing client involvement is behavioral assignments, home practice activities that support the goals of a therapeutic intervention. Behavioral assignments are designed to provide continuity in the treatment of a behavior problem. For example, if an early session with an obese client involved training in self-monitoring. The therapist encourage the client to keep a log of his eating behavior, including the circumstances in which it occurred. Then the therapist and the patient at the next session to plan future behavioral interventions use this log.
- Social Skills and Relaxation Training- Some poor health habits develop in response to the anxiety people experience in social situations. For example, adolescents often begin to smoke to reduce their nervousness in social situations by trying to communicate a cool, sophisticated image. Drinking and overeating may also be responses to social anxiety. Social anxiety can then act as a cue for the maladaptive habit, necessitating an alternative way of coping with the anxiety.
- Relaxation Training- Stressful circumstances cause or maintain many poor health habits, and so managing stress is important to successful behaviour change. A mainstay of stress reduction is relaxation training involving deep breathing and progressive muscle relaxation. In deep breathing, a person takes deep, controlled breaths, which decreases heart rate and blood pressure and increases oxygenation of the blood. People typically engage in deep breathing spontaneously when they feel relaxed. However, in progressive muscle relaxation, an individual learns to relax all the muscles in the body progressively to discharge tension or stress.
- Motivational interviewing- Motivational interviewing (MI) is increasingly used in health promotion interventions. Originally developed to treat addiction, the techniques have been adapted to target smoking, dietary improvements, exercise, cancer screening, and sexual behavior, among other habits (Miller & Rose, 2009). However, motivational interviewing is a client-centered counselling style designed to get people to work through any ambivalence they experience about changing their health behaviors. It may be especially effective for people who are initially wary about whether to change their behavior.
- Relapse Prevention- One of the biggest problems faced in health habit modification is the tendency for people to relapse. Following initial successful behavior change, people often return to their old bad habits. Relapse is a particular problem with the addictive disorders of alcoholism, smoking, drug addiction, and overeating (Brownell, Marlatt, Lichtenstein, & Wilson, 1986), but it can be a problem for all behaviour change efforts.
Evaluation of CBT
The advantages of CBT for health behavior change are several.
- Firstly, a carefully selected set of techniques can deal with all aspects of a problem. Self-observation and self-monitoring define the dimensions of a problem; stimulus control enables a person to modify antecedents of behavior; self-reinforcement controls the consequences of a behavior. And social skills and relaxation training may replace the maladaptive behavior, once brought under some degree of control.
- Second advantage is that it is possible to tailor the therapeutic plan to each individual’s problem. However, each person’s faulty health habit and personality are different. For example the particular package identified for one obese client may not be the same as that developed for another obese client. (Schwartz & Brownell, 1995).
- Third, the range of skills imparted by multimodal interventions may enable people to modify several health habits simultaneously, such as diet and exercise, rather than one at a time (Persky, Spring, Vander Wal, Pagoto, & Hedeker, 2005; Prochaska & Sallis, 2004). Overall, CBT interventions have shown considerable success for a broad array of health behaviors.
Placebo Effect
A placebo is “any medical procedure that produces an effect in a patient because of its therapeutic intent and not its specific nature, whether chemical or physical” (Liberman, 1962, p. 761). The word comes originally from Latin, meaning “I will please.”. Any medical procedure, ranging from drugs to surgery to psychotherapy, can have a placebo effect. Furthermore, Placebo effects extend well beyond the beneficial results of ineffective substances.
Much of the effectiveness of active treatments that produce real cures on their own includes a placebo component. For example, in one study (Beecher, 1959), injected with either morphine or a placebo to the patients complaining of pain. Although morphine was substantially more effective in reducing pain than was the placebo. Not to mention, the placebo was a successful painkiller in 35 percent of the cases.
Placebo effects are enhanced when the physician shows faith in a treatment, the patient is predisposed to believe it will work, these expectations are successfully communicated and the trappings of medical treatment are in place. Placebos are also a vital methodological tool in evaluating drugs and other treatments.
Read More- what are health behaviors?
References
Ogden, J. (2017). Health psychology: A textbook (4th Ed.).McGraw Hill Education.
Taylor, Shelley E. (2018). Health Psychology (10th Ed). McGraw Hill Higher Education. Indian Edition
Subscribe to Careershodh
Get the latest updates and insights.
Join 16,488 other subscribers!
Niwlikar, B. A. (2022, March 25). 13 Important Ways to Change Health Habits. Careershodh. https://www.careershodh.com/how-to-change-health-habits/
