Introduction
Cancer is one of the leading causes of morbidity and mortality worldwide. The World Health Organization (WHO) estimates that one in six deaths globally is due to cancer. Early detection plays a crucial role in improving survival rates and treatment efficacy. However, receiving a cancer diagnosis can be an emotionally devastating experience, making pre-test and post-test counselling essential in helping patients navigate their journey with cancer.
Cancer diagnosis involves a series of tests and procedures aimed at identifying the presence, type, and stage of cancer. Pre-test counselling ensures that individuals undergoing diagnostic procedures are mentally and emotionally prepared, while post-test counselling provides guidance, support, and treatment decision-making assistance.
Read More- Stages of Therapy
Cancer Diagnosis
The diagnosis of cancer involves multiple diagnostic techniques that vary depending on the suspected type of cancer. Below are the primary methods of cancer detection-
1. Imaging Techniques- Imaging is a non-invasive method used to detect tumors and abnormal tissue growth. The most common imaging techniques include-
- X-ray- Often the first diagnostic tool used for detecting lung, bone, or breast cancer.
- Computed Tomography (CT) Scan: Provides cross-sectional images of the body, helping detect tumors in soft tissues and organs.
- Magnetic Resonance Imaging (MRI)- Uses magnetic fields and radio waves to create detailed images, particularly useful for detecting brain and spinal cord tumors.
- Positron Emission Tomography (PET) Scan- Helps in staging cancer by identifying areas of high metabolic activity, indicating tumor growth.
- Ultrasound- Frequently used for detecting tumors in soft tissues such as the liver, kidneys, or ovaries.
2. Biopsy (Gold Standard for Cancer Diagnosis)- A biopsy involves extracting a sample of suspicious tissue or cells for microscopic examination to confirm the presence of cancer. Common biopsy methods include-
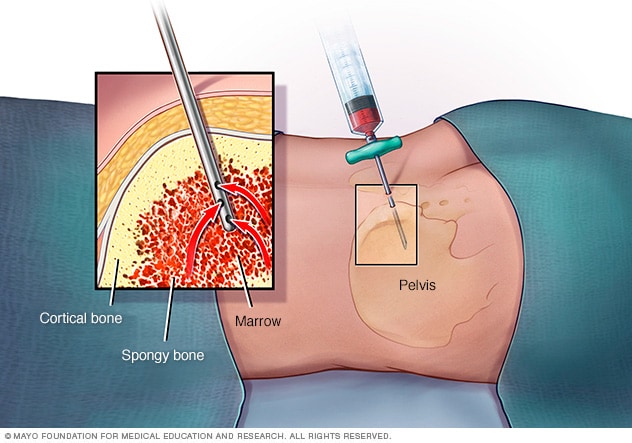
Needle Biopsy
- Needle Biopsy- A fine or core needle is used to extract tissue samples.
- Surgical Biopsy- A larger tissue sample is taken through minor surgery.
- Endoscopic Biopsy- A thin, flexible tube (endoscope) is inserted into the body to collect samples from internal organs.
3. Blood Tests and Tumor Markers- Blood tests help in detecting abnormal markers associated with cancer-
- Complete Blood Count (CBC)- Used to diagnose leukemia and other blood cancers.
- Tumor Markers- Substances produced by cancer cells, such as PSA (for prostate cancer), CA-125 (for ovarian cancer), and AFP (for liver cancer).
4. Genetic Testing- Genetic screening is performed for individuals with a family history of cancer to detect mutations in genes such as BRCA1 and BRCA2 (breast and ovarian cancer risk factors).
5. Endoscopic Examinations- This can include-
Upper Endoscopy
- Colonoscopy- Used for detecting colorectal cancer.
- Bronchoscopy- Used for diagnosing lung cancer.
- Gastroscopy- Used for detecting stomach and esophageal cancers.
Pre-Test Counselling
Pre-test counselling is crucial in helping patients understand the diagnostic process, manage anxiety, and make informed decisions about undergoing tests. The main objectives of pre-test counselling include-
- Providing Clear and Accurate Information- Explaining the purpose, process, benefits, and risks of the test. Clarifying potential outcomes and their implications.
- 2. Addressing Emotional and Psychological Concerns- Many patients experience anxiety, fear, or denial before testing. Counsellors provide emotional support to help patients cope with stress.
- Obtaining Informed Consent- Patients must be fully aware of the risks and benefits before undergoing tests. For genetic testing, implications for family members are discussed.
- Discussing the Possibility of Positive or Negative Result- Patients should be mentally prepared for any outcome. The emotional impact of a positive diagnosis is discussed beforehand.
- Ethical Considerations in Genetic Testing- If genetic testing is conducted, patients are informed about hereditary risks and options for preventive measures. Issues of privacy, discrimination, and confidentiality are addressed.
Read More- Rollo May’s 4 Stages of Personality
Post-Test Counselling
Receiving a cancer diagnosis can lead to shock, anxiety, depression, and uncertainty. Post-test counselling helps patients and families understand the results and make informed decisions regarding treatment.
1. Communicating the Diagnosis- If the results are negative: Patients are reassured and advised on lifestyle modifications for cancer prevention. If the results are positive-
- The type and stage of cancer are explained.
- Treatment options, prognosis, and potential side effects are discussed.
2. Addressing Emotional Reactions- A cancer diagnosis triggers a range of emotions, including-
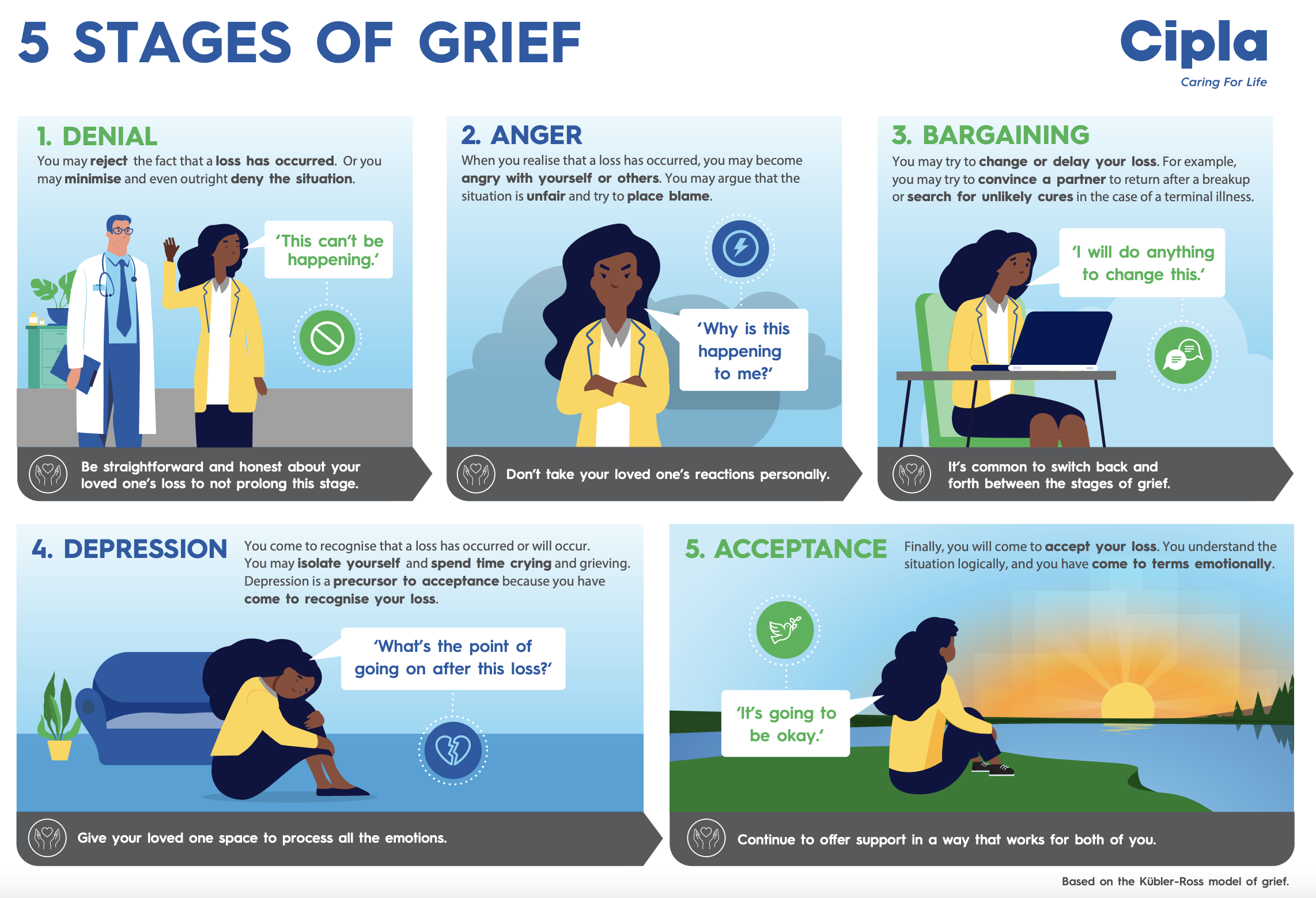
5 Stages of Grief With Cancer
- Denial- “This can’t be happening to me.”
- Anger- “Why me?”
- Depression- Feeling hopeless and overwhelmed.
- Acceptance- Gradual understanding and preparation for treatment.
3. Supporting Treatment Decision-Making- Patients are guided through various treatment options, including-
- Surgery (removal of tumors)
- Chemotherapy (drug treatment)
- Radiotherapy (targeted radiation)
- Immunotherapy (boosting immune response)
- Palliative care (symptom management for advanced cancer)
4. Family and Social Support- Families receive guidance on how to support the patient emotionally and physically. Counsellors help resolve family conflicts related to caregiving responsibilities.
5. Palliative and End-of-Life Care- Patients with advanced cancer are counselled on pain management, hospice care, and psychological well-being. Spiritual and existential concerns are also addressed.
Psychosocial Aspects of Cancer Counselling
Cancer not only affects the body but also mental health and social life. Effective counselling addresses-

Types of Cancer Treatment
- Anxiety and Depression- Studies show that 25-30% of cancer patients experience depression. Therapies such as Cognitive-Behavioral Therapy (CBT) help manage distress.
- Coping Strategies- Techniques like mindfulness, journaling, guided imagery, and relaxation exercises help patients manage stress. Support groups provide encouragement and shared experiences.
- Addressing Survivorship Issues- Cancer survivors often deal with fear of recurrence, physical limitations, and emotional trauma. Counselling helps in reintegrating into daily life and employment.
Conclusion
A cancer diagnosis is life-changing, but with effective pre-test and post-test counselling, patients and their families can navigate the medical and emotional challenges with clarity and support. Proper counselling empowers patients, enhances treatment adherence, and improves overall quality of life. Healthcare professionals must integrate medical expertise with compassionate communication to address both the physical and emotional aspects of cancer care.
References
Faulkner, A. & Maguire, P. (1994). Talking to Cancer Patients and Their Relatives. Oxford University Press.
Kubler-Ross, E. (1969). On Death and Dying. Macmillan.
Kissane, D. W., et al. (1997). Cognitive-Existential Group Therapy for Cancer Patients. Psycho-Oncology, 6, 25-33.
Weisman, A. D. (1985). Thanatology and Psychological Aspects of Dying Patients. Williams & Wilkins.
Niwlikar, B. A. (2025, January 11). Cancer Diagnosis and 5 Important Considerations in Counselling. Careershodh. https://www.careershodh.com/cancer-diagnosis-and-counselling/
