Introduction
The Health Belief Model (HBM) is a psychological framework that was initially developed in the 1950s by social psychologists at the U.S. Public Health Service, notably Irwin M. Rosenstock (1966). This model was created to explain and predict health behaviors by examining individuals’ beliefs and perceptions regarding health risks and potential interventions.
In subsequent decades, Marshall H. Becker and his colleagues expanded the HBM to include additional constructs, enhancing its applicability to various public health issues (Becker, 1974; Becker et al., 1977). The model has been widely applied in health promotion initiatives, including vaccination programs, cancer screenings, smoking cessation efforts, and chronic disease management (Becker & Rosenstock, 1984).
Core Components of the Health Belief Model
The HBM suggests that an individual’s likelihood of engaging in health-related behaviors is influenced by six primary constructs-
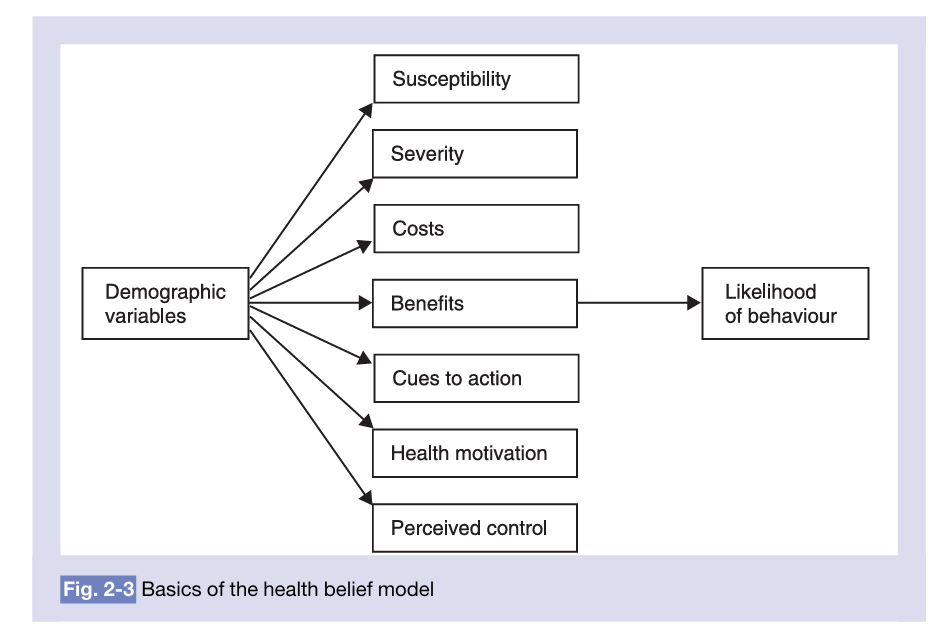
Health Belief Model
- Perceived Susceptibility- This component refers to an individual’s belief about their personal risk of developing a disease or health condition. Research indicates that people who perceive themselves as highly susceptible to a disease are more likely to adopt preventive measures (Rosenstock, 1974). For example, a smoker who believes they are at a high risk of developing lung cancer may be more motivated to quit smoking.
- Perceived Severity- This reflects the belief about the seriousness of a disease and its potential consequences, including physical, emotional, and social impacts. If an individual believes that contracting a disease could lead to severe health issues or even death, they are more likely to engage in preventive behaviors (Becker & Maiman, 1975). For instance, someone who understands the fatal nature of untreated hypertension may be more inclined to adhere to prescribed medication.
- Perceived Benefits- This refers to an individual’s assessment of the advantages of adopting a health-related behavior. When individuals believe that a particular action will reduce their risk of illness or improve their well-being, they are more likely to engage in that behavior (Janz & Becker, 1984). For example, individuals who recognize that regular exercise reduces their risk of cardiovascular diseases are more likely to incorporate it into their routine.
- Perceived Barriers- These are the potential obstacles that individuals perceive when considering a health behavior change, such as financial costs, inconvenience, or discomfort. If the perceived barriers outweigh the benefits, individuals are less likely to take action (Rosenstock, 1974). For example, people may avoid getting flu vaccines due to fears of side effects or accessibility issues.
- Cues to Action- Cues to action are triggers that prompt individuals to engage in health behaviors. These triggers can be internal (such as experiencing symptoms) or external (such as media campaigns, doctor recommendations, or peer influence) (Becker & Rosenstock, 1984). For instance, a public health campaign emphasizing the dangers of skin cancer may prompt individuals to start using sunscreen.
- Self-Efficacy- Introduced later by Bandura (1977) and incorporated into the HBM, self-efficacy refers to an individual’s confidence in their ability to take action successfully. People with high self-efficacy are more likely to overcome barriers and maintain long-term behavioral changes (Becker & Rosenstock, 1984). For example, a person who believes they can successfully quit smoking is more likely to attempt and sustain smoking cessation efforts.

Health Belief Model for Using or Not Using Hearing Aids
Applications of the Health Belief Model
Over the years, the HBM has been applied to various public health interventions and health-related behaviors-
- Vaccination Uptake- Research indicates that individuals who perceive themselves at high risk (perceived susceptibility) and believe in the severity of diseases are more likely to accept vaccinations (Janz & Becker, 1984). For instance, during the COVID-19 pandemic, health campaigns emphasized the risks of the virus and the benefits of vaccination to encourage uptake.
- Cancer Screening Behavior- Several studies have shown that women who perceive themselves as highly susceptible to cervical cancer are more likely to undergo Pap smear screenings (Becker et al., 1977). Similarly, mammography screening behavior has been linked to perceived risk and benefits among women (Champion & Skinner, 2008).
- Smoking Cessation- HBM-based interventions have been used to encourage smoking cessation by emphasizing the risks of smoking-related diseases and highlighting the benefits of quitting (Becker, 1974). Programs often use cues to action such as warning labels on cigarette packages and anti-smoking advertisements.
Read More- Healthy Behaviour

Health Belief Model and Related Intervention Strategies
Criticism of the HBM
Despite its effectiveness in explaining health behaviors, the HBM has faced several criticisms-
- Overemphasis on Rational Decision-Making- One major limitation is that the HBM assumes individuals make rational, logical decisions based on risk assessment. However, research has shown that emotions such as fear, denial, and optimism bias play a significant role in health behavior decision-making (Norman & Fitter, 1989). For example, some smokers downplay the risks of smoking despite knowing the health consequences.
- Limited Consideration of Social and Economic Influences- Unlike other models, such as the Theory of Planned Behavior (TPB), the HBM does not fully account for social and environmental factors, such as peer pressure, cultural norms, and financial barriers (Schwarzer, 1992). This limitation makes it less effective in addressing behaviors influenced by social determinants of health, such as obesity or substance abuse.
- Static Nature of the Model- The HBM does not consider how beliefs change over time, making it less adaptable for long-term behavioral interventions (Becker & Rosenstock, 1987). In reality, individuals’ perceptions of health risks and benefits evolve based on experiences, new information, and changing life circumstances.
Conclusion
The Health Belief Model (HBM) remains one of the most widely used frameworks for predicting and understanding health behaviors. Its structured approach helps public health professionals design effective interventions by addressing individuals’ perceptions of risk, benefits, and barriers.
Despite its limitations, the model provides valuable insights into health decision-making processes. Future research should focus on integrating social, psychological, and emotional factors to enhance the model’s predictive power (Schwarzer, 1992). Additionally, incorporating longitudinal studies to track changes in beliefs over time could improve its applicability in long-term health behavior change strategies.
References
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215.
Becker, M. H. (1974). The health belief model and personal health behavior. Health Education Monographs, 2, 324–473.
Becker, M. H., & Maiman, L. A. (1975). Sociobehavioral determinants of compliance with health and medical care recommendations. Medical Care, 13(1), 10–24.
Becker, M. H., Haefner, D. P., Kasl, S. V., Kirscht, J. P., Maiman, L. A., & Rosenstock, I. M. (1977). Selected psychosocial models and correlates of individual health-related behaviors. Medical Care, 15(5), 27–46.
Becker, M. H., & Rosenstock, I. M. (1984). Compliance with medical advice. Handbook of Health, Health Care, and the Health Professions, 71–110.
Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health Education Quarterly, 11(1), 1–47.
Norman, P., & Fitter, M. (1989). The role of affective beliefs in predicting intentions to quit smoking. Health Education Research, 4(3), 361–368.
Schwarzer, R. (1992). Self-efficacy in the adoption and maintenance of health behaviors: Theoretical approaches and a new model. Self-Efficacy: Thought Control of Action, 217–243.
Subscribe to Careershodh
Get the latest updates and insights.
Join 13,996 other subscribers!
Niwlikar, B. A. (2025, March 3). Health Belief Model and Its 6 Important Components. Careershodh. https://www.careershodh.com/health-belief-model/
